Type 2 Diabetes Mellitus, Self-Care, Adult
Caring for yourself after you have been diagnosed with type 2 diabetes (
type 2 diabetes mellitus) means keeping your blood sugar (
glucose) under control with a balance of:
What are the risks?
Having type 2 diabetes can put you at risk for other long-term (chronic) conditions, such as heart disease and kidney disease. Your health care provider may prescribe medicines to help prevent complications from diabetes.
How to monitor your blood glucose

-
Check your blood glucose every day or as often as told by your health care provider.
-
Have your A1C (hemoglobin A1C) level checked two or more times a year, or as often as told by your health care provider.
- Your health care provider will set personalized treatment goals for you. Generally, the goal of treatment is to maintain the following blood glucose levels:
How to manage hyperglycemia and hypoglycemia
Hyperglycemia symptoms
Hyperglycemia, also called high blood glucose, occurs when blood glucose is too high. Make sure you know the early signs of hyperglycemia, such as:
Hypoglycemia symptoms
Hypoglycemia, also called low blood glucose, occurs with a blood glucose level at or below 70 mg/dL (3.9 mmol/L). Diabetes medicines lower your blood glucose and can cause hypoglycemia. The risk for hypoglycemia increases during or after exercise, during sleep, during illness, and when skipping meals or not eating for a long time (fasting).
It is important to know the symptoms of hypoglycemia and treat it right away. Always have a 15-gram rapid-acting carbohydrate snack with you to treat low blood glucose. Family members and close friends should also know the symptoms and understand how to treat hypoglycemia, in case you are not able to treat yourself. Symptoms may include:
Hunger.
Anxiety.
Sweating and feeling clammy.
Dizziness or feeling light-headed.
Sleepiness.
Increased heart rate.
Irritability.
Tingling or numbness around the mouth, lips, or tongue.
Restless sleep.
Severe hypoglycemia is when your blood glucose level is at or below 54 mg/dL (3 mmol/L).
Severe hypoglycemia is an emergency. Do not wait to see if the symptoms will go away. Get medical help right away. Call your local emergency services (911 in the U.S.). Do not drive yourself to the hospital.
If you have severe hypoglycemia and you cannot eat or drink, you may need glucagon. A family member or close friend should learn how to check your blood glucose and how to give you glucagon. Ask your health care provider if you need to have an emergency glucagon kit available.
Follow these instructions at home:
Medicines
-
Take prescribed insulin or diabetes medicines as told by your health care provider.
-
Do not run out of insulin or other diabetes medicines. Plan ahead so you always have these available.
-
If you use insulin, adjust your dosage based on your physical activity and what foods you eat. Your health care provider will tell you how to adjust your dosage.
-
Take over-the-counter and prescription medicines only as told by your health care provider.
Eating and drinking
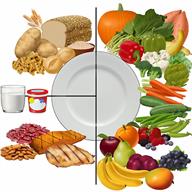
What you eat and drink affects your blood glucose and your insulin dosage. Making good choices helps to control your diabetes and prevent other health problems. A healthy meal plan includes eating lean proteins, complex carbohydrates, fresh fruits and vegetables, low-fat dairy products, and healthy fats.
Make an appointment to see a registered dietitian to help you create an eating plan that is right for you. Make sure that you:
Follow instructions from your health care provider about eating or drinking restrictions.
Drink enough fluid to keep your urine pale yellow.
Keep a record of the carbohydrates that you eat. Do this by reading food labels and learning the standard serving sizes of foods.
Follow your sick-day plan whenever you cannot eat or drink as usual. Make this plan in advance with your health care provider.
Activity
- Stay active. Exercise regularly, as told by your health care provider. This may include:
-
When you start a new exercise or activity, work with your health care provider to adjust your insulin, medicines, or food intake as needed.
Lifestyle
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
- If you drink alcohol and your health care provider says that it is safe for you:
- Limit how much you have to:
Know how much alcohol is in your drink. In the U.S., one drink equals one 12 oz bottle of beer (355 mL), one 5 oz glass of wine (148 mL), or one 1½ oz glass of hard liquor (44 mL).
-
Learn to manage stress. If you need help with this, ask your health care provider.
Take care of your body

- Keep your immunizations up to date. In addition to getting vaccinations as told by your health care provider, it is recommended that you get vaccinated against the following illnesses:
-
Schedule an eye exam soon after your diagnosis, and then one time every year after that.
-
Check your skin and feet every day for cuts, bruises, redness, blisters, or sores. Schedule a foot exam with your health care provider once every year.
-
Brush your teeth and gums two times a day, and floss one or more times a day. Visit your dentist one or more times every 6 months.
-
Maintain a healthy weight.
General instructions
-
Share your diabetes management plan with people in your workplace, school, and household.
-
Carry a medical alert card or wear medical alert jewelry.
-
Keep all follow-up visits. This is important.
Questions to ask your health care provider
For help and guidance and for more information about diabetes, please visit:
Summary
-
Caring for yourself after you have been diagnosed with type 2 diabetes (type 2 diabetes mellitus) means keeping your blood sugar (glucose) under control with a balance of nutrition, exercise, lifestyle changes, and medicine.
-
Check your blood glucose every day, as often as told by your health care provider.
-
Having diabetes can put you at risk for other long-term (chronic) conditions, such as heart disease and kidney disease. Your health care provider may prescribe medicines to help prevent complications from diabetes.
-
Share your diabetes management plan with people in your workplace, school, and household.
-
Keep all follow-up visits. This is important.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.