ThisiscontentfromElsevier'sDrugInformation
Vitamin D
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
General dosing information
NOTE: Individuals with increased risk for vitamin D deficiency (e.g., chronic fat malabsorption disorders, people with chronic kidney disease, people living with HIV, or people taking certain enzyme-inducing medications, etc.) may require higher supplemental doses than those recommended for healthy individuals to maintain normal vitamin D status.[36895] [52900] [59376] 25(OH)D concentrations can be used to guide adequate dietary supplementation.
20 mcg/day (800 International Units/day) PO.[71565]
15 mcg/day (600 International Units/day) PO.[71565]
15 mcg/day (600 International Units/day) PO.[71565]
10 mcg/day (400 International Units/day) PO is the recommended Adequate Intake. No RDA has been established.[71565]
10 mcg/day (400 International Units/day) PO is the recommended Adequate Intake. No RDA has been established.[71565]
10 mcg/day (400 International Units/day) PO is the recommended Adequate Intake.[52900] [54484] [62270] Doses up to 20 mcg/day (800 International Units/day) have been used in preterm infants.[70608] [70609] No RDA has been established.[71565]
5 to 10 mcg/day (200 to 400 International Units/day) PO.[54484] No RDA has been established.[71565]
20 to 50 mcg (800 to 2,000 International Units) PO once daily. Adjust dosage to maintain serum 25-hydroxyvitamin D concentrations of 30 ng/mL or more. Max: 250 mcg/day (10,000 International Units/day).[66596]
20 to 50 mcg (800 to 2,000 International Units) PO once daily. Adjust dosage to maintain serum 25-hydroxyvitamin D concentrations of 30 ng/mL or more. Max: 250 mcg/day (10,000 International Units/day).[66596]
20 to 25 mcg (800 to 1,000 International Units) PO once daily. Adjust dosage to maintain serum 25-hydroxyvitamin D concentrations of 30 ng/mL or more. Max: 100 mcg/day (4,000 International Units/day).[66596]
10 to 12.5 mcg (400 to 500 International Units) PO once daily. Adjust dosage to maintain serum 25-hydroxyvitamin D concentrations of 30 ng/mL or more. Max: 50 mcg/day (2,000 International Units/day).[66596]
10 to 12.5 mcg (400 to 500 International Units) PO once daily. Adjust dosage to maintain serum 25-hydroxyvitamin D concentrations of 30 ng/mL or more. Max: 50 mcg/day (2,000 International Units/day).[66596]
50 mcg (2,000 International Units) PO once daily.[69099]
50 mcg (2,000 International Units) PO once daily.[69099]
75 mcg (3,000 International Units) PO once daily until serum vitamin D concentration is more than 30 ng/mL.[69358]
NOTE: In adults, the Institute of Medicine (IOM) defines vitamin D deficiency as 25(OH)D concentrations of 30 nmol/L or less (12 ng/mL or less) and vitamin D insufficiency as 25(OH)D concentrations of 30 to 50 nmol/L (12 to less than 20 ng/mL). Generally all persons are sufficient at levels of 50 nmol/L or more (20 ng/mL or more).[31730] [52900] In pediatric patients, the American Academy of Pediatrics (AAP) and the IOM define vitamin D deficiency as 25(OH)D concentrations of 37.5 nmol/L or less (15 ng/mL or less) and vitamin D insufficiency as 25(OH)D concentrations of 50 nmol/L or less (20 ng/mL or less).[36919] [52900] [59376] In contrast, the Endocrine Society guidelines for adults and pediatric patients define vitamin D insufficiency as 25(OH)D concentrations less than 75 nmol/L (less than 30 ng/mL) and vitamin D deficiency as 25(OH)D concentrations less than 50 nmol/L (less than 20 ng/mL).[62269]
150 mcg (6,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO once weekly for at least 8 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 25 to 50 mcg (1,000 to 2,000 International Units) PO once daily. Maintenance doses of 1,250 mcg (50,000 International Units) PO once monthly have also been used. Individualize dose based on serum vitamin D concentrations.[62269] [68414] [68416] [69357] [70601]
50 to 150 mcg (2,000 to 6,000 International Units) PO once daily or 350 to 1,250 mcg (14,000 to 50,000 International Units) PO once weekly for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 15 to 25 mcg (600 to 1,000 International Units) PO once daily.[36919] [62269] [66854] [66855] [69395] [69396] Maintenance doses of 1,250 mcg (50,000 International Units) PO once monthly have also been used.[68414] Individualize dose based on serum vitamin D concentrations.
25 to 125 mcg (1,000 to 5,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO once weekly for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 10 to 25 mcg (400 to 1,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[36919] [62269] [69395] [69396]
25 to 50 mcg (1,000 to 2,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO once weekly for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 10 to 25 mcg (400 to 1,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[36919] [62269] [69395] [69396]
40 to 150 mcg (1,600 to 6,000 International Units) PO once daily, initially. May increase the dose to a maximum of 250 mcg (10,000 International Units) PO once daily to maintain a serum vitamin D concentration of at least 30 ng/mL (75 mmol/L).[66596]
40 to 150 mcg (1,600 to 6,000 International Units) PO once daily, initially. May increase the dose to a maximum of 250 mcg (10,000 International Units) PO once daily to maintain a serum vitamin D concentration of at least 30 ng/mL (75 mmol/L).[66596]
40 to 75 mcg (1,600 to 3,000 International Units) PO once daily, initially. May increase the dose to a maximum of 100 mcg (4,000 International Units) PO once daily to maintain a serum vitamin D concentration of at least 30 ng/mL (75 mmol/L).[66596]
20 to 25 mcg (800 to 1,000 International Units) PO once daily, initially. May increase the dose to a maximum of 50 mcg (2,000 International Units) PO once daily to maintain a serum vitamin D concentration of at least 30 ng/mL (75 mmol/L).[66596]
20 to 25 mcg (800 to 1,000 International Units) PO once daily, initially. May increase the dose to a maximum of 50 mcg (2,000 International Units) PO once daily to maintain a serum vitamin D concentration of at least 30 ng/mL (75 mmol/L).[66596]
75 to 250 mcg (3,000 to 10,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO 1 to 3 times weekly to achieve a serum vitamin D concentration more than 30 ng/mL, then 75 to 150 mcg (3,000 to 6,000 International Units) PO once daily.[62269] [69358]
150 to 250 mcg (6,000 to 10,000 International Units) PO once daily (2 to 3 times the usual recommended dose) to achieve a serum vitamin D concentration more than 30 ng/mL, then 30 to 75 mcg (1,200 to 3,000 International Units) PO once daily.[62269]
150 to 250 mcg (6,000 to 10,000 International Units) PO once daily (2 to 3 times the usual recommended dose) to achieve a serum vitamin D concentration more than 30 ng/mL, then 20 to 75 mcg (800 to 3,000 International Units) PO once daily.[62269]
100 to 150 mcg (4,000 to 6,000 International Units) PO once daily (2 to 3 times the usual recommended dose) to achieve a serum vitamin D concentration more than 30 ng/mL, then 20 to 75 mcg (800 to 3,000 International Units) PO once daily.[62269]
50 to 500 mcg (2,000 to 20,000 International Units) PO daily for 4 to 8 weeks, with the duration of treatment determined by evidence of radiologic healing. Thereafter, supplement with the RDA to prevent further deficiency.[52884] [52946] Alternatively, at least 125 mcg (5,000 International Units) PO once daily has also been recommended for initial treatment; weekly regimens (e.g., high doses, such as 1,250 mcg [50,000 International Units] PO once weekly) or a single higher-dose course over 1 to 5 days may be considered if compliance is an issue that prevents adequate repletion.[36919] [53381] Large single dose regimens (5,000 to 15,000 mcg [200,000 to 600,000 International Units] PO divided into 2 to 4 doses administered over 1 day) have been used when compliance is a concern, but are sometimes controversial due to a purported risk for hypercalcemia. It is important to ensure adequate dietary intake of calcium and phosphorus.[52884] [52946] Active treatment may continue for 2 to 3 months to replete deficient stores, followed by maintenance dosing with the RDA.[36919] Individualize dose based upon 25(OH)D concentrations.[52884]
25 to 125 mcg (1,000 to 5,000 International Units) PO once daily has been recommended. Radiologic evidence of healing is usually observed in 2 to 4 weeks, and the active treatment duration is usually 2 to 3 months, after which the supplementation may be reduced to maintenance dosing in accordance with RDAs to prevent further deficiency. Supplementation with calcium is necessary due to the risk of hypocalcemia during bone remineralization.[36919] It is important to ensure adequate dietary intake of calcium and phosphorus.[52884] [52946] Weekly regimens (e.g., high doses, such as 1,250 mcg [50,000 International Units] PO once weekly) have been considered in older infants if compliance is an issue that prevents adequate repletion.[36919] [53381] Individualize dose based upon 25(OH)D concentrations.[52884]
25 mcg (1,000 International Units) PO once daily has been recommended. Radiologic evidence of healing is usually observed in 2 to 4 weeks, and the active treatment duration is usually 2 to 3 months, after which the supplementation may be reduced to maintenance dosing in accordance with RDAs to prevent further deficiency. Supplementation with calcium is necessary due to the risk of hypocalcemia during bone remineralization.[36919] It is important to ensure adequate dietary intake of calcium and phosphorus.[52884] [52946] Individualize dose based upon 25(OH)D concentrations.[52884]
Treatment for HVDRR is not standardized. Despite significant improvements in vitamin D concentrations following high-dose ergocalciferol (or use of a vitamin D analog like calcitriol) alone, patients may remain hypocalcemic and hypophosphatemic. High doses of ergocalciferol (vitamin D2) have been used in these patients. The following regimens have been used with variable results: 100 to 1,000 mcg/day (4,000 to 40,000 International Units/day) PO or 5 to 7 mcg/kg/day (200 to 280 International Units/kg/day) PO. However, doses as high as 5,000 mcg/day (200,000 International Units/day) PO have not been effective in improving the disease in other patients. Patients should receive a 3 to 6 month trial of high dose vitamin D along with high-dose calcium therapy. Patients without alopecia appear more likely to respond.[52884] [52947] The FDA-approved dose is 300 to 12,500 mcg (12,000 to 500,000 International Units) PO daily. Calcium intake should be adequate. Blood calcium and phosphorus determinations are recommended every 2 weeks or more frequently if clinically indicated. X-rays of the bones are recommended every month until condition is corrected and stabilized.[30166] Individualize dose based upon 25(OH)D concentrations.[52884]
20 to 25 mcg (800 to 1,000 international units) PO daily is recommended by the National Osteoporosis Foundation. Supplementation regimen should include calcium for greatest benefit.[67144]
20 mcg (800 International Units) PO daily; different doses may be recommended dependent on concomitant pharmacological treatment or prevention. The American College of Rheumatology recommends supplementation of vitamin D and calcium in all patients receiving corticosteroid therapy, especially if treatment duration will exceed 3 months.[44888]
20 mcg (800 International Units) PO daily. The American College of Rheumatology recommends supplementation of vitamin D and calcium in all patients receiving corticosteroid therapy, especially if treatment duration will exceed 3 months.[44888]
A total dose of 17.5 mcg (700 International Units) PO daily from a combination of dietary and non-dietary sources. In a population-based study of 3,025 females, the daily vitamin D and calcium intake was followed to determine if vitamin D or calcium had an impact on the risk of developing PMS. Women with the highest intake of vitamin D from both dietary sources and supplements (median 17.7 mcg [706 International Units daily]) had a reduced risk of developing PMS compared with those women with the lowest intake of vitamin D of 2.8 mcg (112 International Units) daily (RR of 0.59, 95% CI 0.4 to 0.86, p = 0.01 for the trend).[31641]
1,250 to 5,000 mcg (50,000 to 200,000 International Units) PO once daily along with calcium supplements.[30166]
1,250 to 5,000 mcg (50,000 to 200,000 International Units) PO once daily along with calcium supplements.[30166]
150 mcg (6,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO once weekly for at least 8 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 25 to 50 mcg (1,000 to 2,000 International Units) PO once daily or 1,250 mcg (50,000 International Units) PO once monthly.[62269] [66587] [66588] [66589] [66590] [68416] [69357] [70601] Individualize dose based on serum vitamin D concentrations. Cholecalciferol is more effective at raising serum total 25-hydroxyvitamin D concentrations in non-dialysis-dependent CKD patients (CKD G3a-5) compared with ergocalciferol and may be preferable in these patients.[66588] [66589] [66590]
200 mcg (8,000 International Units) PO once daily for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 25 to 50 mcg (1,000 to 2,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[58204] [62269] [68414] [70603] Cholecalciferol is more effective at raising serum total 25-hydroxyvitamin D concentrations in non-dialysis-dependent CKD patients (CKD G3a-5) compared with ergocalciferol and may be preferable in these patients. [66588] [66589] [66590] [70603]
100 mcg (4,000 International Units) PO once daily for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 25 to 50 mcg (1,000 to 2,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[58204] [62269] [68414] [70603] Cholecalciferol is more effective at raising serum total 25-hydroxyvitamin D concentrations in non-dialysis-dependent CKD patients (CKD G3a-5) compared with ergocalciferol and may be preferable in these patients.[66588] [66589] [66590] [70603]
50 mcg (2,000 International Units) PO once daily for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 25 to 50 mcg (1,000 to 2,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[58204] [62269] [68414] [70603] Cholecalciferol is more effective at raising serum total 25-hydroxyvitamin D concentrations in non-dialysis-dependent CKD patients (CKD G3a-5) compared with ergocalciferol and may be preferable in these patients.[66588] [66589] [66590] [70603]
25 to 50 mcg (1,000 to 2,000 International Units) PO once daily for at least 6 weeks to achieve a serum vitamin D concentration more than 30 ng/mL, then 10 to 25 mcg (400 to 1,000 International Units) PO once daily. Individualize dose based on serum vitamin D concentrations.[58204] [62269] [68414] [70603] Cholecalciferol is more effective at raising serum total 25-hydroxyvitamin D concentrations in non-dialysis-dependent CKD patients (CKD G3a-5) compared with ergocalciferol and may be preferable in these patients.[66588] [66589] [66590] [70603]
20 to 30 mcg (800 to 1,200 International Units) PO once daily has been recommended. Alternative regimen is 15,000 mcg (600,000 International Units) PO once every 2 months. If vitamin D supplementation is started early, it prevents development of osteopenia in these patients.[53313]
20 to 30 mcg (800 to 1,200 International Units) PO once daily has been recommended. Alternative regimen is 2,500 mcg (100,000 International Units) PO once every 2 months. If vitamin D supplementation is started early, it prevents development of osteopenia in these patients.[53313]
Serum 25(OH)D concentrations are recommended for monitoring vitamin D status because it is reflective of both sources of vitamin D, sunlight and dietary. It is not, however, reflective of vitamin D body stores.[52900] Circulating 1,25(OH)2D is not a good indicator of vitamin D status due to its shorter half-life and its tight regulation by parathyroid hormone, calcium, and phosphorus. Levels of 1,25(OH)2D do not usually decrease until severe vitamin D deficiency.[52879]
The Institute of Medicine recommends the following regarding the interpretation of 25(OH)D concentrations and vitamin D status for normal healthy persons:[52900]
Maintenance Tolerable Upper Intake Level (UL) is 100 mcg/day (4,000 International Units/day) PO.
Maintenance Tolerable Upper Intake Level (UL) is 100 mcg/day (4,000 International Units/day) PO.
Maintenance Tolerable Upper Intake Level (UL) is 100 mcg/day (4,000 International Units/day) PO.
Children 9 to 12 years: Maintenance Tolerable Upper Intake Level (UL) is 100 mcg/day (4,000 International Units/day) PO.
Children 4 to 8 years: Maintenance Tolerable Upper Intake Level (UL) is 75 mcg/day (3,000 International Units/day) PO.
Children 1 to 3 years: Maintenance Tolerable Upper Intake Level (UL) is 62.5 mcg/day (2,500 International Units/day) PO.
Infants 7 to 12 months: Maintenance Tolerable Upper Intake Level (UL) is 37.5 mcg/day (1,500 International Units/day) PO.
Infants 1 to 6 months: Maintenance Tolerable Upper Intake Level (UL) is 25 mcg/day (1,000 International Units/day) PO.
Maintenance Tolerable Upper Intake Level (UL) is 25 mcg/day (1,000 International Units/day) PO.
Specific guidelines for dosage adjustments in hepatic impairment are not available; higher doses may be needed to compensate for reductions in intestinal absorption.
Specific guidelines for dosage adjustments in renal impairment are not available. However, vitamin D is activated in the kidney; close monitoring is required to ensure the appropriate dose.
† Off-label indication

















Vitamin D is a fat-soluble vitamin and has two primary forms: cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2). The chemical structure differences between the two forms of vitamin D do not affect the metabolism or clinical responses once activated within the body. Although animal experiments have indicated a difference in toxicity between vitamin D3 and vitamin D2, human studies have been inconclusive. Vitamin D is available in dietary supplements as ergocalciferol or cholecalciferol and is also found in fortified milk and cereal products; liver, fish liver oils, fatty fish, and egg yolks from hens have also been supplemented with vitamin D. Vitamin D must undergo hydroxylation in the liver and kidney to its active form. Vitamin D is responsible for appropriate calcium and phosphate balance and is required for normal bone growth and mineralization. Vitamin D status is determined by monitoring 25-hydroxyvitamin D [25(OH)D] serum concentrations, which represent all sources of vitamin D (e.g., sunlight and dietary or from supplements). Although labeled for use in several disease states, the primary use is for vitamin D supplementation and the prevention and treatment of vitamin D deficiency and rickets.[52900]
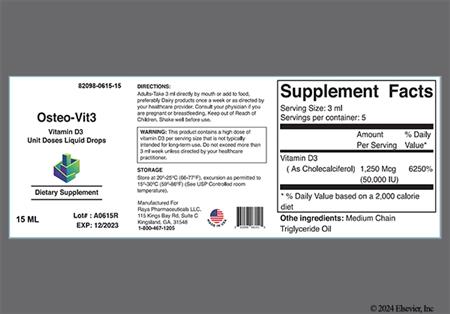
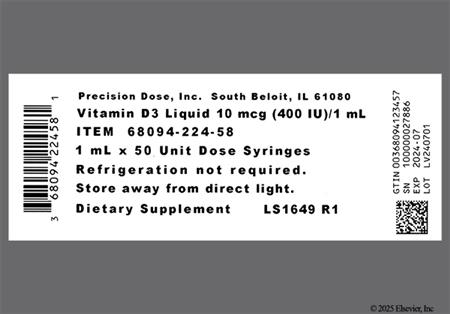
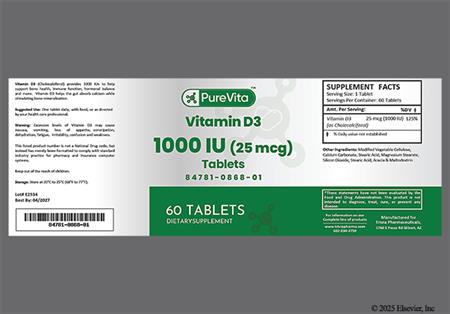
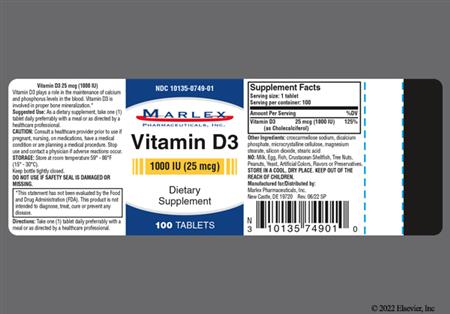
For storage information, see the specific product information within the How Supplied section.
In general, the use of supplemental vitamin D according to recommended dietary intakes is not associated with serious adverse reactions. Vitamin D may cause side effects in overdose, but such symptoms associated with hypervitaminosis D (and resultant hypercalcemia) are rarely reported. An excess of vitamin D causes abnormally high levels of calcium in the blood and is almost always caused by vitamin D analogs (e.g., calcitriol, doxercalciferol, paricalcitol), rather than vitamin D found in dietary supplements (e.g., cholecalciferol, ergocalciferol). However, patients taking higher doses of vitamin D supplements should report any of the following potential signs of high vitamin D/calcium concentrations: nausea/vomiting, constipation, loss of appetite, increased thirst (polydipsia), increased urinary frequency, mental/mood changes or irritability, headache, unusual fatigue or tiredness. These symptoms may require clinical evaluation. Anorexia, weight loss, polyuria, and arrhythmias may also be observed. In addition, hypercalcemia due to bone resorption leading to hypercalciuria may be observed in prolonged hypervitaminosis D. In early stages of vitamin D toxicity, hypercalcemia is mild and renal function remains normal. As vitamin D toxicity continues, continued bone resorption and increased calcium levels lead to suppression of parathyroid production. Calcification of the vasculature and other tissues has been associated with prolonged vitamin D toxicity. Data do not support that vitamin D toxicity is associated with kidney stones. Death due to vitamin D intoxication is likely due to renal and cardiovascular failure. Long-term doses of vitamin D of 250 to 1,000 mcg/day (10,000 to 40,000 International Units/day) and long-term serum 25(OH)D concentrations of 500 to 600 nmol/L (200 to 400 ng/mL) are associated with vitamin D toxicity. Symptoms of vitamin D toxicity can become apparent within 4 weeks of continual excessive ingestion. Due to the long half-life of vitamin D, symptoms of toxicity may be prolonged. Excessive sun exposure does not result in vitamin D toxicity.[52900] [30166]
Risk of growth inhibition in infants due to vitamin D supplements is based on a 1938 report of 35 infants up to 45 weeks of age where high-dose vitamin D supplementation (45 to 112.5 mcg/day [1,800 to 4,500 International Units/day] for 6 months) was associated with growth inhibition in comparison with lower dose vitamin D supplements (less than 8.5 mcg/day [340 International Units/day] for 6 months). In a subsequent but smaller study (n = 11) performed in 1966, no association between vitamin D supplements and growth inhibition was found. However, due to a possible association, no RDI for vitamin D has been set for infants.[52900] A large observational study from Finland in 2011 reported no association between growth inhibition later in life (as evaluated at 14 and 31 years of age) and the administration of vitamin D supplements (50 mcg/day [2,000 International Units/day]) during infancy.[52948]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Certain vitamin D formulations may contain FD&C Yellow No. 5 (tartrazine), a dye that can cause allergic-type reactions in susceptible individuals. While the overall incidence of tartrazine sensitivity is low in the general population, it occurs more frequently in patients with aspirin hypersensitivity.[30166]
Some formulations of vitamin D, such as ergocalciferol capsules, are contraindicated in patients with malabsorption syndromes.[30166] In these patients, higher doses of vitamin D are necessary, and cholecalciferol is preferred due to its superior bioavailability and more predictable absorption profile.[66596]
Vitamin D is contraindicated in patients with hypercalcemia or hypervitaminosis D. Hypersensitivity to vitamin D is one etiologic factor in infants with idiopathic hypercalcemia; in these patients, vitamin D intake must be seriously restricted.[30166] [66856] Some formulations of the oral solution (e.g., ergocalciferol oral drops) contain propylene glycol. Clinicians should be aware of the toxic potential in young children, including premature neonates, term neonates, infants, and children younger than 4 years, and ensure an appropriate formulation is selected. Excessive exposure to propylene glycol may result in lactic acidosis, hyperosmolality, tachypnea, tachycardia, diaphoresis, and central nervous system toxicity, including seizures and intraventricular hemorrhage.[36919] [72468]
Patients with renal impairment or renal failure may be at increased risk for vitamin D-induced hypercalcemia even with usual dosages. Close clinical monitoring is needed to ensure adequate supplementation and, in pediatric patients, proper growth. In patients with stage 3 or higher kidney disease, use of a vitamin D analog appears preferred, following recommendations of the National Kidney Foundation.[38437] [52900]
Adverse effects have not been reported with the normal daily intake of Vitamin D within the recommended dietary daily intakes for a pregnant female. Animal reproduction studies have shown fetal abnormalities in several species associated with hypervitaminosis D; therefore, the use of vitamin D in excess of the recommended dietary allowance during normal pregnancy should be avoided unless, in the judgment of the physician, potential benefits outweigh the hazards involved.[30166] The RDA of vitamin D during pregnancy is 15 mcg/day (600 International Units/day) with a Tolerable Upper Intake Limit of 100 mcg/day (4,000 International Units/day).[52900]
The 25-hydroxyvitamin D metabolite of vitamin D is distributed into human breast milk at concentrations relative to the maternal serum concentration. Typical breast milk concentrations (without maternal supplementation) are not sufficient to prevent vitamin D deficiency in infants that are exclusively breast-fed and do not receive other vitamin D supplementation. Prolonged, exclusive breast-feeding of infants without recommended vitamin D supplementation is a significant cause of rickets in infants, especially in dark-skinned infants breast-fed by mothers who are not vitamin D replete.[52900] Use of vitamin D within the recommended daily dietary intake for lactating women is generally recognized as safe.[31028] The recommended maternal daily allowance of vitamin D during breast-feeding is 600 International Units/day with a Tolerable Upper Intake Limit of 4000 International Units/day.[52900] While high-dose vitamin D supplementation to nursing mothers has been shown to increase the concentration of vitamin D in breast milk and favorably increase 25(OH)D levels in infants, the results have not been validated and supplementation to infants is still recommended.[36895] Generally, the serum calcium concentrations of the infant should be monitored when a nursing mother is prescribed vitamin D in high doses, since hypercalcemia has been reported with high dose maternal use.[30166]
Use vitamin D supplements with caution in patients with sarcoidosis due to the increased risk of hypercalcemia.[54025]
Both forms of vitamin D are metabolized to the active form, calcitriol (1,25-dihydroxyvitamin D); all vitamin D activity is due to this metabolite. Calcitriol promotes renal reabsorption of calcium, increases intestinal absorption of calcium and phosphorus, and increases calcium mobilization from bone to plasma. Calcitriol promotes intestinal absorption of calcium through binding to a specific receptor in the mucosal cytoplasm of the intestine. Subsequently, calcium is absorbed through formation of a calcium-binding protein. The synthesis of calcitriol is enhanced by elevated parathyroid hormone levels and low plasma phosphorus levels. Hypocalcemia causes release of parathyroid hormone, which stimulates the production of calcitriol.[52900]
The vitamin D receptor (VDR) is present in numerous tissues throughout the body; the exact action of calcitriol within these tissues is not completely understood. There is evidence that calcitriol plays a role in the immune system. Calcitriol has been shown to inhibit cancer growth and stimulate cell differentiation.[52900]
Revision Date: 10/08/2025, 01:31:00 AMVitamin D is administered orally. Maximal clinical effects of a given dosage are usually observed in 4 weeks. Dietary vitamin D is absorbed from the GI tract in the presence of bile salts and is initially bound to chylomicrons, then is slowly transferred to vitamin D binding protein (DBP) in the serum. The uptake by chylomicrons results in vitamin D update by adipose tissue and muscle; remaining vitamin D in circulation is then metabolized by the liver. The uptake by the liver and other tissues accounts results in a plasma half-life of 4 to 6 hours for supplemental vitamin D. However, studies have shown that the whole-body half-life is about 2 months due to the stores in these tissues.[52879]
Ergocalciferol and cholecalciferol are considered prohormones and are converted in the liver by a group of activating cytochrome P450 (CYP) enzymes, CYP2R1, CYO27A1, and CYP27B1, to 25-hydroxyvitamin D (25(OH)D, calcidiol), the predominant form of vitamin D in the blood. This metabolite has a half-life of about 15 days. Serum 25(OH)D concentrations increase in a non-linear fashion in response to increased vitamin D intake based on baseline concentrations and duration of supplementation. Increasing serum 25(OH)D levels to more than 50 nmol/L requires a greater amount of vitamin D than increasing baseline levels that are less than 50 nmol/L. The impact on serum 25(OH)D concentrations is less when doses are at least 25 mcg/day (1,000 International Units/day) compared to doses less than 25 mcg/day (1,000 International Units/day). For example, for vitamin D doses of at least 25 mcg/day (1,000 International Units/day), the increase in serum 25(OH)D concentrations is about 1 nmol/L for each 1 mcg (40 International Units) of vitamin D. Conversely, for vitamin D doses of 15 mcg (600 International Units) or less, the increase in 25(OH)D concentrations is about 2.3 nmol/L for each 1 mcg (40 International Units) of vitamin D.[52900] In the kidneys, 25-hydroxyvitamin D is further converted to its active, hormonal form, 1,25-dihydroxyvitamin D (1,25(OH)2D, calcitriol), which has a half-life of about 15 hours and accounts for only a small portion of the total body amount of vitamin D. Synthesis to this active form by renal CYP27B1 is tightly regulated by parathyroid hormone and serum phosphate levels.[52879] [52900] All metabolites of vitamin D are excreted through the bile into the feces; very little is excreted in the urine.
Vitamin D is well absorbed orally in most individuals without conditions associated with fat malabsorption. There is a time lag of 10 to 24 hours between the oral administration of vitamin D and the initiation of its action in the body due to the necessity of synthesis of the active metabolites in the liver and kidneys.[30166]
Vitamin D absorption can be decreased in patients with any hepatic disease associated with fat malabsorption.[62269]
Of relevance to breastfed children, the 25-hydroxyvitamin D metabolite is distributed into maternal breast milk; however, the concentration in breast milk is dependent upon the maternal serum concentration. Typical breast milk concentrations of vitamin D without maternal vitamin D supplementation are less than 0.625 to 1.95 mcg/L (25 to 78 International Units/L); these levels of vitamin D will not be sufficient to prevent vitamin D deficiency in infants who are exclusively breastfed. Administration of high-dose vitamin D supplementation to nursing mothers has been shown to increase the concentration of vitamin D in breast milk and favorably increase 25(OH)D levels in infants; however, the results have not been validated and supplementation to infants is still recommended.[36895]
Persons with body mass index (BMI) of 30 or more have lower 25(OH)D levels as compared to those with a lower BMI. In addition, people who are obese may require higher doses of vitamin D to achieve 25(OH)D levels comparable to non-obese people. The increased amounts of subcutaneous fat in these persons sequester more vitamin D and alter its release into the circulation. Also, obese patients who have undergone gastric bypass surgery will become vitamin D deficient over time without sufficient supplementation, since part of the small intestine where vitamin D is absorbed is bypassed and vitamin D mobilization from fat stores will not compensate over time.[52900]
Biliary or GI Disease
Vitamin D absorption can be decreased in patients with any biliary or GI disease that results in fat malabsorption.[62269]
Adverse effects have not been reported with the normal daily intake of Vitamin D within the recommended dietary daily intakes for a pregnant female. Animal reproduction studies have shown fetal abnormalities in several species associated with hypervitaminosis D; therefore, the use of vitamin D in excess of the recommended dietary allowance during normal pregnancy should be avoided unless, in the judgment of the physician, potential benefits outweigh the hazards involved.[30166] The RDA of vitamin D during pregnancy is 15 mcg/day (600 International Units/day) with a Tolerable Upper Intake Limit of 100 mcg/day (4,000 International Units/day).[52900]
The 25-hydroxyvitamin D metabolite of vitamin D is distributed into human breast milk at concentrations relative to the maternal serum concentration. Typical breast milk concentrations (without maternal supplementation) are not sufficient to prevent vitamin D deficiency in infants that are exclusively breast-fed and do not receive other vitamin D supplementation. Prolonged, exclusive breast-feeding of infants without recommended vitamin D supplementation is a significant cause of rickets in infants, especially in dark-skinned infants breast-fed by mothers who are not vitamin D replete.[52900] Use of vitamin D within the recommended daily dietary intake for lactating women is generally recognized as safe.[31028] The recommended maternal daily allowance of vitamin D during breast-feeding is 600 International Units/day with a Tolerable Upper Intake Limit of 4000 International Units/day.[52900] While high-dose vitamin D supplementation to nursing mothers has been shown to increase the concentration of vitamin D in breast milk and favorably increase 25(OH)D levels in infants, the results have not been validated and supplementation to infants is still recommended.[36895] Generally, the serum calcium concentrations of the infant should be monitored when a nursing mother is prescribed vitamin D in high doses, since hypercalcemia has been reported with high dose maternal use.[30166]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.