ThisiscontentfromElsevier'sDrugInformation
Influenza Virus Vaccine
Learn more about Elsevier’s Drug Information today! Get the reliable drug data and decision support you need to enhance patient safety through timely and accessible information.
General Dosing Information
0.5 mL IM as a single dose.[51849]
0.5 mL IM as a single dose.[63436]
0.5 mL IM as a single dose.[30823]
0.5 mL IM as a single dose.[30823]
0.5 mL IM. For children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.5 mL IM at least 4 weeks after the initial dose.[30823] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.25 mL or 0.5 mL IM. For infants and children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.25 mL or 0.5 mL IM at least 4 weeks after the initial dose.[30823] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.5 mL IM as a single dose.[60361]
0.5 mL IM as a single dose.[63436]
0.5 mL IM as a single dose.[41685]
0.5 mL IM as a single dose.[41685]
0.5 mL IM. For infants and children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.5 mL IM at least 4 weeks after the initial dose.[41685] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.5 mL IM as a single dose.[47301]
0.5 mL IM as a single dose.[47301]
0.5 mL IM. For infants and children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.5 mL IM at least 4 weeks after the initial dose.[47301] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.5 mL IM as a single dose.[41448]
0.5 mL IM as a single dose.[41448]
0.5 mL IM. For children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.5 mL IM at least 4 weeks after the initial dose.[41448] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.25 mL IM. For infants and children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.25 mL IM at least 4 weeks after the initial dose.[41448] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.5 mL IM as a single dose.[52415]
0.5 mL IM as a single dose.[52415]
0.5 mL IM. For children who have not received at least 2 doses of influenza vaccine before the beginning of the influenza season, administer a second dose of 0.5 mL IM at least 4 weeks after the initial dose.[52415] The Advisory Committee on Immunization Practices (ACIP) recommends that infants and children aged 6 months through 8 years who have previously received at least 2 doses of influenza vaccine before the beginning of the influenza season, receive only 1 dose for the current influenza season. The 2 previous doses need not have been given during the same season or consecutive seasons.[63436]
0.5 mL IM as a single dose.[52915]
0.5 mL IM as a single dose.[52915]
0.1 mL intradermally as a single dose.[58656]
0.5 mL/dose IM; 0.1 mL/dose intradermal (Fluzone Intradermal only). Safety and efficacy of Fluad and Fluzone High-Dose have not been established.
0.5 mL/dose IM. Safety and efficacy of intradermal administration have not been established.
0.5 mL/dose IM for Fluzone, Fluarix, FluLaval, Afluria (excluding the needle-free injection system), Flucelvax and Flublok. Safety and efficacy of Fluzone High-Dose, Fluad, and intradermal administration have not been established.
9 to 12 years: 0.5 mL/dose IM for Fluzone, Fluarix, FluLaval, Afluria (excluding the needle-free injection system), Flucelvax and Flublok. Safety and efficacy of Fluzone High-Dose, Fluad, and intradermal administration have not been established.
3 to 8 years: 0.5 mL/dose IM for Fluzone, Fluarix, FluLaval, Afluria (excluding the needle-free injection system), and Flucelvax. Safety and efficacy of Fluzone High-Dose, Flublok, Fluad, and intradermal administration have not been established.
1 to 2 years: 0.25 mL/dose IM for Afluria (excluding the needle-free injection system); 0.5 mL/dose IM for FluLaval, Fluarix, Fluzone, and Flucelvax. Safety and efficacy of Fluzone High-Dose, Flublok, Fluad, and intradermal administration have not been established.
6 to 11 months: 0.25 mL/dose IM for Afluria (excluding the needle-free injection system); 0.5 mL/dose IM for Flulaval, Fluarix, Fluzone, and Flucelvax. Safety and efficacy of Fluzone High-Dose, Flublok, Fluad, and intradermal administration have not been established.
1 to 5 months: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication

















NOTE: The 2025/2026 trivalent inactivated vaccine virus strains for egg-based vaccines are an A/Victoria/4897/2022 (H1N1) pdm09-like virus, an A/Croatia/10136RV/2023 (H3N2)-like virus, and a B/Austria/1359417/2021 (B/Victoria lineage)-like virus. The trivalent formulation of cell- or recombinant-based influenza vaccines are an A/Wisconsin/67/2022 (H1N1) pdm09-like virus, an A/District of Columbia/27/2023 (H3N2)-like virus, and a B/Austria/1359417/2021 (B/Victoria lineage)-like virus.[72015]
Inactivated influenza virus vaccine (IIV) is used to confer immunity against specific strains of influenza virus. Most IIV products consist of inactivated virus particles prepared from the allantoic fluid of chick embryos inoculated with the influenza virus; however, some egg-free products are now available. Flucelvax employs mammalian cells (Madin-Darby canine kidney epithelial cells) rather than chicken embryos to prepare the inactivated virus particles.[52415] Flublok uses baculovirus (Autographa californica nuclear polyhedrosis virus) infected insect cells (fall armyworm) to produce recombinant influenza virus hemagglutinin (HA) proteins.[52915] Because influenza viruses are continually changing and antibodies produced by the host in response to the vaccine diminish over time, annual immunization is required. The parenteral influenza vaccines contain either 3 (2 type A and 1 type B) or 4 (2 type A and 2 type B) strains that represent the influenza viruses likely to circulate during the annual flu season. The US and Canadian governments (individually) determine annually which strains to include in the vaccine based on epidemiological studies and consultation with several groups, including the World Health Organization.[63436] The Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) recommend annual flu vaccination with an age-appropriate influenza vaccine, without preference of 1 product or formulation over another, for everyone 6 months and older.[63436][63520]
Updates for coronavirus disease 2019 (COVID-19):
The influenza season will coincide with the continued or recurrent circulation of SARS-CoV-2. Influenza vaccination of patients 6 months and older may reduce symptoms that might be confused with those of COVID-19. Additionally, prevention and reduction of influenza severity could decrease hospitalizations and intensive care unit admissions and alleviate stress on the health care system.[63436]
For storage information, see the specific product information within the How Supplied section.
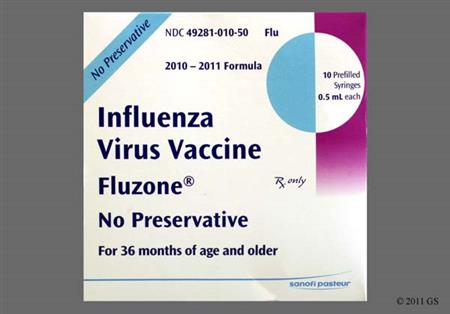
Fluzone
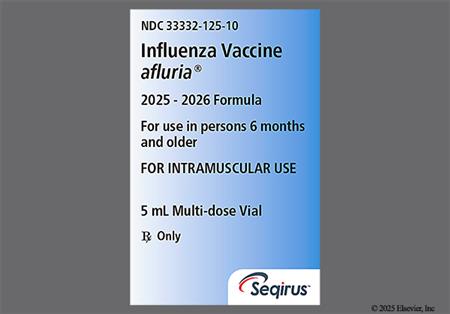
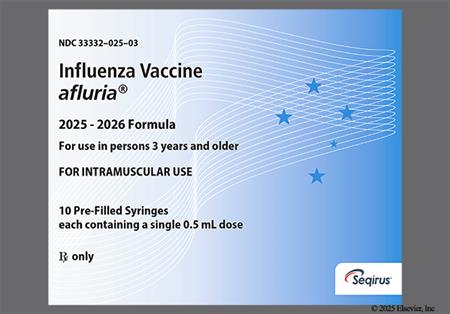
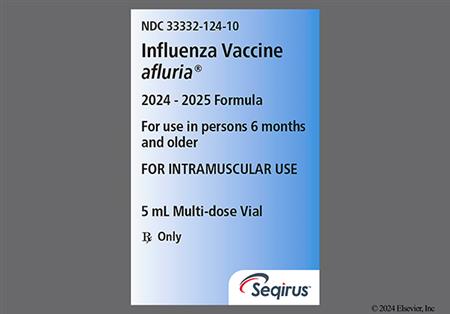
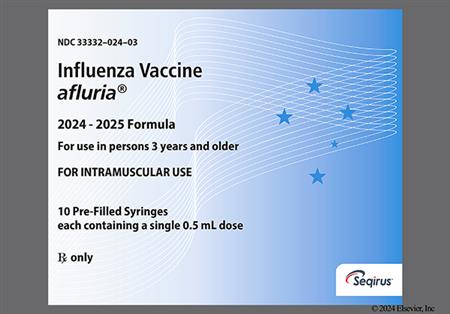
Afluria
Intradermal administration (Fluzone Intradermal only)
Adverse reactions associated with administration of the influenza virus vaccine are usually mild and are more likely to occur in children than in adults. The most common adverse reaction occurring after influenza virus vaccine is an injection site reaction that can manifest as pain (more than 1%), erythema (more than 1%), tenderness (21% to 77.9%), induration (0.5% to 17.7%), swelling (0.5% to 56.8%), pruritus (0.2% to 46.9%), or ecchymosis (0.5% to 17%).[30823] [41448] [41685] [47301] [51849] [52415] [52915] [60361] [64726] Extensive swelling of the injected limb has been reported with postmarketing use of Flucelvax.[52415] In older adults, 23% reported some type of injection site reaction as compared with 14% of those given placebo. This study also revealed that reactions were more frequent in women than men, although the reason for this was unclear.[23572] Among adults who received Afluria vaccine, 36% to 69% had local tenderness, 15% to 48% had pain, 3% to 16% had erythema (redness), 4% to 9% had swelling, and 5% or less had bruising at the injection site. Of the adults (18 to 64 years) administered Afluria via the PharmaJet Stratis needle-free injection system, 89% had local tenderness, 65% had swelling, 64% had pain, 60% had erythema (redness), 28% had pruritus, and 18% had bruising. In studies including pediatric patients (5 to 17 years of age) receiving Alfuria Quadrivalent, 45.2% to 51.3% had pain, 14.8% to 19.4% had erythema (redness), and 10.7% to 15.5% had swelling. In children 6 to 59 months of age, pain (20.8% to 35.5%), redness (20.8% to 22.4%), and swelling/lump (6.1% to 10.1%) were the most frequently reported injection site reactions.[41448] Local injection site reactions occurred in more patients at least 65 years of age after Fluzone High-Dose than after Fluzone. For example, pain was reported in 35.6% of the Fluzone High-Dose recipients whereas 24.3% of Fluzone recipients experienced pain. Further, erythema and swelling were experienced more frequently in the Fluzone High-Dose (14.9% and 8.9%) compared to Fluzone recipients (10.8% and 5.8%).[51849] In pediatric patients 6 months to 8 years receiving Fluzone, 57% to 66% had pain, 47.3% to 54.1% had tenderness, 23.1% to 37.3% had erythema, and 12.9% to 24.8% had swelling.[30823] In individuals (9 to 64 years) who received Flublok, pain (32% to 40.2%) was the most common injection-site reaction. In individuals 65 years and older receiving Flublock, pain was reported at 19%.[52915] Injection site abscess and injection site cellulitis has been reported with influenza virus vaccine during postmarketing experience.[41685] Adverse local reactions typically persist for up to 2 days.
Systemic adverse reactions such as malaise (1% to 38.1%), drowsiness (13% to 37.7%), fever (0% to 16%), diaphoresis (1% to 10%), arthralgia (0.3% to 15%), chills (1.4% to 7.3%), shivering (2.6% to 12.1%), fatigue (1% to 21%), headache (1% to 26%), and/or myalgia (1% to 35.5%) can occur after administration of the influenza virus vaccine.[30823] [41448] [41685] [41686] [47301] [51849] [52415] [52915] [58656] [60361] [64726] Of the adults (18 to 64 years) administered Afluria via the PharmaJet Stratis needle-free injection system, 36% had myalgia, 31% had malaise, 25% had headache, 7% had chills, and less than 1% had fever.[41448] These reactions generally begin 6 to 12 hours after administration of the vaccine and persist for 1 to 2 days. Children who have not been previously exposed to influenza virus are more likely to experience these reactions, especially if administered the whole-virus vaccine. It is recommended that children receive the split-virus (subvirion) vaccines instead of whole-virus immunizations. In fact, placebo-controlled trials suggest that among older adults and healthy young adults, split-virus influenza vaccine is not associated with higher rates of systemic symptoms than placebo injections. More patients at least 65 years of age who received Fluzone High-Dose as compared with Fluzone had systemic adverse reactions. For example, among Fluzone High-Dose and Fluzone recipients, 21.4% vs. 18.3% had myalgia, 18% vs. 14% had malaise, 16.8% vs. 14% had headache, and 3.6% vs. 2.3% had fever.[51849] Similarly, more patients at least 65 years of age who received Fluad as compared with Agriflu had systemic adverse reactions. Older adults receiving Fluad experienced myalgia (14.7% vs. 9.7% Agriflu), fatigue (13.3% vs. 10.4% Agriflu), headache (13.2% vs. 11.2% Agriflu), arthralgia (8.5% vs. 7.8% Agriflu), and chills (6.7% vs. 4.7% Agriflu).[60361] Irritability (1.7% to 32.9%), malaise and fatigue (1% to 14.3%), myalgia (9.9%), headache (6.2%), and fever (3.7% to 7.2%) were reported in pediatric patients 6 to 59 months of age after receiving Afluria. Irritability was reported in 16% to 21% of pediatric patients after receiving Fluarix.[41685] [52652] Irritability (34.9% to 54%) and abnormal crying (18.6% to 41.2%) were also reported in pediatric patients 6 to 36 months of age after receiving Fluzone.[30823] Migraine was reported in 1% of adult patients after receiving Fluarix.[41685] In adult individuals (18 years and older) receiving Flublok, headache (10% to 23%), malaise and fatigue (13% to 16.5%), muscle pain/myalgia (8% to 20.3%), chills (3% to 6.3%), arthralgia (4% to 8%), and fever (3% or less) were reported. Myalgia (19.3%), headache (18.5%), malaise (16.1%), chills (7.3%), and fever (2.8%) were reported in pediatric patients (9 to 17 years) receiving Flublok during clinical trials.[52915] Chills, asthenia, feeling hot, and abnormal gait have been observed during postmarketing surveillance.[41686] [47301]
Rarely, immediate allergic reactions occur after inactivated influenza vaccine administration. An allergic reaction may present as urticaria, angioedema, bronchospasm, or anaphylactoid reactions including anaphylaxis or anaphylactic shock; these reactions are most likely the result of hypersensitivity to residual egg protein. In 4 clinical trials of trivalent inactivated influenza vaccine with more than 10,000 subjects, 1 case of anaphylaxis occurred.[52652] Facial swelling was reported in 1% of adults receiving influenza virus vaccine during clinical trials.[47301] Erythema multiforme, rash, vesicular rash, maculopapular rash, pruritus, serum sickness, and Stevens-Johnson syndrome have been reported with inactivated influenza vaccine through postmarketing surveillance.[30823] [41448] [41685] [41686] [47301] [51849] [52415] [52915] [60361] [64726]
An increased risk of developing the Guillain-Barre syndrome (GBS) after administration of the inactivated influenza virus vaccine was evident in 1976. Subsequent influenza vaccinations during the next few years were not associated with this increased risk. However, during 1993 to 1994 twice the average yearly rate (for the period 1990 to 1995) of influenza vaccine-associated incidences of GBS were reported, representing a risk of slightly more than 1 additional case of GBS per million persons vaccinated. In most cases, symptoms were limited and reversible, but fatalities have occurred. Persons with a history of GBS have a substantially greater likelihood of subsequently developing GBS than persons without such a history. Thus, the likelihood of coincidentally developing GBS after influenza vaccination is expected to be greater among persons with a history of GBS than among persons with no history of this syndrome. It is not known if influenza vaccination is causally associated with this risk for recurrence of GBS. GBS has been reported with influenza virus vaccine during postmarketing surveillance.[30823] [41448] [41685] [41686] [47301] [51849] [52415] [52915] [60361] [64726]
Neurological disorders temporally associated with influenza vaccination, such as encephalopathy, optic neuritis/neuropathy, partial facial muscle paralysis, and neuropathic pain in the area of the brachial plexus, have been reported. Hypoesthesia, hypokinesia, abnormal gait, tremor, myelitis (including encephalomyelitis and transverse myelitis), confusion, dizziness, vertigo, insomnia, neuralgia, facial and cranial nerve paralysis, facial palsy (Bell's palsy), and limb paralysis have been reported with influenza virus vaccine in postmarketing surveillance.[41448] [41685] [47301] [51849] [52415] [52915] [60361] [64726]
Microscopic polyangiitis, Henoch-Schonlein purpura, and vasculitis, including vasculitis which may be associated with transient renal involvement, have been reported with postmarketing experience using influenza virus vaccine.[30823] [41448] [41685] [41686] [47301] [60361] [64726]
Febrile seizures have been temporally associated with administration of the inactivated influenza vaccine (IIV). As of December 13, 2010, there were 53 confirmed VAERS reports of febrile seizures in children 6 to 23 months of age after receiving any 2010 to 2011 IIV; 42 of these cases occurred after vaccination with Fluzone (trivalent IIV). The majority of seizures (32 of the 42) were classified as non-serious, and all patients recovered. Of the 42 reports, 36 occurred on the same day or the day after vaccination (median time between vaccination and seizure onset was 10 hours), and 27 received Fluzone at the same time as other vaccines. The elevation in temperature ranged from 100.4 to 104 degrees F.[43210] Over a 3 year period from 2003 to 2006, 35 seizures were reported after influenza vaccination. Seizures occurred in the presence of fever in 21 of the 35 reports, and 29 of the 35 occurred within 2 weeks of vaccination. Five of the 35 seizures occurred in patients with a history of prior seizures.[43209] During the 2006 to 2007 through 2010 to 2011 influenza seasons, increases in reports of febrile seizures occurred in children 6 months to 23 months of age receiving the IIV and PCV7, PCV13, or DTaP-containing vaccines. During the 2014 to 2015 season, administration of IIV with PCV13 also resulted in an increased risk for febrile seizures within days 0 to 1 after vaccine co-administration. Although this observational data may suggest association of the seizure with the simultaneous administration of the vaccines, immunization should not be delayed (e.g., by separating administration across multiple healthcare visits) due to the threat of disease.[47234] [63436] Convulsions (including febrile seizures) have been reported during postmarketing experience.[51849] [61129] [64726]
Respiratory adverse reactions that have occurred after administration of influenza virus vaccine include rhinitis (1% to 10%), rhinorrhea (2.7% to 11.2%), nasal congestion (1% to 7%), otitis media (1.6% to 2.4%), nasopharyngitis (1% to 5%), infectious croup (1.4%), influenza-like illness (1% to 1.6%), cough (more than 1%), sore throat (more than 1%), teething (1.3%), upper respiratory tract infection (more than 1%), pharyngitis (more than 1%), oropharyngeal pain (more than 1%), and wheezing (1%).[30823] [41448] [41685] [41686] [47301] [52415] [52915] Dyspnea, dysphonia, stridor, respiratory distress, laryngitis, bronchospam, throat tightness, and asthma have been reported with influenza virus vaccine through postmarketing surveillance.[41685] [47301] [51849] [64726]
Gastrointestinal adverse reactions that have occurred after administration of influenza virus vaccine include anorexia (loss of appetite) (1% to 32.3%), vomiting (0% to 14.8%), nausea (0.4% to 12%), change in eating habits (10% to 17.4%), upper abdominal pain (1.4%), and diarrhea (1% to 24.2%).[30823] [41448] [41685] [41686] [47301] [52415] [52915] [60361] Dysphagia has been reported with influenza virus vaccine in postmarketing surveillance.[47301]
Neck pain, dysmenorrhea (1.3%), back pain (1.5%), and pain in extremity (1.2%) have been reported in adults after administration of influenza virus vaccine (Fluarix).[41685] Arthritis and muscle weakness have been reported with influenza virus vaccine through postmarketing surveillance.[47301]
Thrombocytopenia and lymphadenopathy have been reported with influenza virus vaccine through postmarketing surveillance.[30823] [41448] [41685] [41686] [47301] [51849] [60361] [64726]
Red eyes (4% to 7%) have been reported in adult patients after administration of inactivated influenza vaccine. Conjunctivitis, photophobia, ocular pain, ocular inflammation, eyelid swelling, eye swelling, eye irritation, optic neuritis/neuropathy, and conjunctival hyperemia have been reported with influenza virus vaccine through postmarketing surveillance.[30823] [41685] [47301] [51849] [64726]
Chest tightness was reported in 3% of adults receiving influenza virus vaccine during clinical trials.[47301] Chest pain (unspecified), sinus tachycardia, pallor, and flushing have been reported with influenza virus vaccine in postmarketing surveillance.[41685] [47301] [51849] [64726]
Injectable vaccines, including the influenza virus vaccine, have been associated with episodes of syncope and fainting. These events may be accompanied by transient tonic-clonic limb movements, visual disturbances, and paresthesias. Prior to administration, ensure procedures are in place to prevent falls and restore cerebral perfusion. Monitor vaccine recipients after administration of the dose. If syncope occurs, place the patient in a supine or Trendelenburg position to restore cerebral perfusion.[30823] [41685] [47301] [51849] [52415] [52915] [60361] [64726]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Egg-based vaccines contain trace egg protein and may rarely cause anaphylaxis, but the Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), the American Academy of Allergy, Asthma, and Immunology (AAAAI), and the American College of Allergy, Asthma, and Immunology (ACAAI) do not recommend any special precautions for egg-allergic recipients. For individuals with a history of severe allergic reactions (e.g., anaphylaxis) to an influenza vaccine, recommendations vary based on the specific vaccine previously implicated and if an alternative formulation can be used safely under medical supervision.[63436][62809][63436][63520] Flucelvax and Flublok are not egg-propagated and are contraindicated only in persons with severe reaction to that vaccine or its components.[52415][52915] Use caution when administering the inactivated influenza vaccine (IIV) to patients with gelatin hypersensitivity because gelatin may be used in some formulations of the IIV as a stabilizer.[56390][56391]
Deferral of the influenza virus vaccine administration may be appropriate for a patient with a moderate or severe acute illness such as infection with or without fever. The Advisory Committee on Immunization Practices recommends that vaccinations be delayed during the course of a moderate or severe acute febrile illness and administered after the acute phase of illness has resolved. All vaccines can be administered to persons with minor illnesses such as diarrhea, mild upper-respiratory infection with or without low-grade fever, or other low-grade febrile illness. Vaccinate persons with moderate or severe febrile illness as soon as they have recovered from the acute phase of the illness.[65107]
The influenza virus vaccine should be used with caution in patients who have experienced a history of significant adverse event(s) associated with previous use. Carefully consider the potential benefits and risks of the inactivated influenza vaccine (IIV) for patients who have developed Guillain-Barre syndrome (GBS) within 6 weeks of a previous influenza vaccination. Influenza immunization is generally not recommended in patients who have developed GBS within 6 weeks of a previous influenza vaccination. However, for most persons with a history of GBS who are at high risk for severe complications from influenza, many experts believe the benefits of the influenza virus vaccine justify yearly vaccination.[41448] [41685] [47301] [51849] [52415] [52915] [53026] [60361] [63436] [64726] [65107]
Influenza virus vaccine is compatible with breast-feeding. The Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) state inactivated virus vaccines pose no risk for breast-feeding individuals or their children. Additionally, breast-feeding does not adversely affect immunization; limited data suggest breast-feeding may enhance the immune response to certain vaccine antigens. There are no available data regarding the presence of the influenza virus vaccine in human milk, its effects on the breastfed child, or its effects on milk production. No adverse effects have been reported in children potentially exposed to influenza virus vaccine through breast milk.[30823] [41448] [41685] [47301] [52415] [52915] [63436] [65107] [70365] [71393]
If the influenza virus vaccine is administered to immunosuppressed individuals, including those receiving immunosuppressive therapy, the immune response may be lower than in immunocompetent individuals.[30823] [41448] [41685] [47301] [51849] [52415] [52915] [60361] [64726] Although the influenza virus vaccine may be less effective in patients with significant immunosuppression, influenza incidence and severity is higher in this patient population; therefore, vaccination with the influenza virus vaccine is recommended for these patients. Patients with primary immunodeficiency includes patients with severe combined immunodeficiency (SCID), hypogammaglobulinemia, or agammaglobulinemia. The effectiveness of any vaccine is uncertain when it depends on humoral response. Individuals with human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS) may have a diminished immune response, influenza incidence and severity is higher in this patient population; therefore, administer the influenza virus vaccine according to the routine vaccine schedule. Vaccination with influenza virus vaccine is recommended during chemotherapy and radiation therapy, although vaccination with other vaccines should be avoided due to potential suboptimal antibody response. Allogeneic stem cell transplant patients who received the influenza virus vaccine prior to hematopoietic stem cell transplant (HSCT) should receive repeat influenza virus vaccine doses routinely after HSCT. Administer the influenza virus vaccine at least 6 months after HSCT and annually thereafter. Patients may be vaccinated as early as 4 months after HSCT; however, a second dose should be considered.[65107] The influenza virus vaccine may be given as early as 1 month post solid organ transplant, but should be avoided during active treatment for rejection.[67938]
No adequate and well-controlled studies have been conducted in pregnant individuals. Based on available data from pregnancy registries of Flucelvax and Fluarix administered during pregnancy, there was no evidence of vaccine-associated risk of major birth defects or miscarriage.[41685] [52415] Data from a post-licensure observational, retrospective safety surveillance study showed no evidence of a vaccine-associated increase in the risk of birth defects and miscarriages when Flublok quadrivalent is administered during pregnancy.[52915] Data from a Pregnancy Exposure Registry in the U.S. looked at individuals vaccinated with Afluria quadrivalent vaccine during the influenza season 2017 to 2018 through 2020 to 2021. Of 483 pregnancies, 477 resulted in live births with 485 infants born. There were 2 stillbirths, neither with major birth defects (1 patient was vaccinated in the first trimester and 1 patient was vaccinated during the second trimester). There were 160 patients vaccinated before 20 weeks gestation, in these patients there were 4 spontaneous abortions (2.5%). Among the 171 patients vaccinated in the first trimester, there were 2 major birth defects (1.2%). In the 201 patients vaccinated in the second trimester, there were 2 major birth defects (1%). The data generated from this registry demonstrates rates of miscarriage and major birth defects that are consistent with the estimated background rates.[61129] During animal studies, no evidence of impaired fertility or fetal harm was noted with influenza vaccines. Pregnancy may increase the risk of serious medical complications from influenza. Therefore, the Advisory Committee on Immunization Practices (ACIP) recommends that all individuals who are or will be pregnant (in any trimester) during the influenza season be routinely vaccinated with an inactivated influenza vaccine (vs. live-attenuated influenza vaccine).[41685] [63436] The American College of Obstetricians and Gynecologist (ACOG) committee also recommends pregnant individuals receive the inactivated or recombinant influenza vaccine as soon as it becomes available. Ideally, the influenza vaccine should be given by the end of October in the United States, but vaccination during flu season can occur at anytime. It is safe and effective to administer other non-virus containing or inactive vaccines (Tdap, RSV, or Covid-19 vaccine) during the same visit.[70419] In addition to benefits to the pregnant person, influenza vaccine administration during pregnancy appears to help protect newborns and infants. Fewer cases of laboratory-confirmed influenza occurred during the first 6 months of life among infants of the 159 mothers who received the inactivated influenza vaccine (6 cases) as compared with infants of 157 mothers who received the pneumococcal polysaccharide vaccine (16 cases). Some manufacturers have established pregnancy registries to monitor pregnancy outcomes and newborn health after vaccination. Individuals who receive these vaccines during pregnancy are encouraged to enroll in these registries. Individuals who receive Flublok during pregnancy are encouraged to call 1-800-822-2463 or complete information online at https://www.sanofipasteurpregnancyregistry.com.[30823] [41448] [41685] [47301] [52415] [52915] [71393]
Influenza virus vaccine imparts immunity against the influenza virus by stimulating production of antibodies that are specific to the disease. Vaccine recipients develop immunity only to those strains of the virus from which the vaccine was prepared. Influenza viruses are recognized by the surface antigens they carry, and two such antigens, hemagglutinin (H) and neuraminidase (N) have been identified and are used to classify the various viruses. Subtypes of these strains (H1, H2, H3, N1, N2) are associated with influenza A virus and have been recognized to cause disease in humans. Immunity to these surface antigens increases resistance to infection and decreases the severity of the disease if infection occurs. Eventually, antigenic variation can occur, and immunity to one strain may no longer impart immunity to distantly related subtypes of the virus. Influenza B viruses also exhibit antigenic variation, and new variants of both types of viruses continue to cause widespread epidemics of respiratory disease.[61129]
Revision Date: 09/10/2025, 01:32:00 AMThe inactivated influenza virus vaccine (IIV) is usually administered intramuscularly; intradermal vaccines are also available. The vaccine usually imparts a protective effect within 10 to 14 days of administration. Post-vaccine antibody titers are generally high enough in healthy young adults and children to provide resistance against infection by strains found in the vaccine as well as related strains. A hemagglutination-inhibiting antibody titer of at least 1:40 may be protective against influenza infection in up to 50% of people. Among 1,077 patients 18 to 64 years of age who got Afluria, 94.2 to 99.9% had a postvaccination titer of at least 1:40. The duration of immunity imparted by the influenza vaccine generally lasts 6 to 12 months.[61129]
Infants and Children 6 to 47 months
Three clinical studies evaluated the immunogenicity of Fluvirin in healthy patients (n = 285) and those at increased risk for influenza complications (n = 41). Patients at increased risk were vaccinated with two 0.25 mL doses. After vaccination, 49% or more demonstrated at least a 4-fold increase in HI antibody titers to all strains, with titers of 1:40 or more in 71% or more of patients. A lower immune response was demonstrated for Fluvirin in 2 clinical studies when the vaccine was compared to 2 other spilt vaccines in patients 6 to 47 months of age, with the greatest differences demonstrated in those less than 36 months of age. Due to these differences, Fluvirin must only be used in patients 4 years of age or older.[41686]
Infants and Children 6 months to 8 years
The immunogenicity of Fluzone was evaluated in a multi-center study during which 68 infants and children 6 to 35 months of age were given 2 doses of 0.25 mL 26 days apart and 120 children 3 to 8 years were given 2 doses of 0.5 mL 30 days apart. Influenza vaccine was given during the previous flu season to 54.4% of those in the 6 to 35 months age group and 27.5% in the 3 to 8 years age group. One month after the last dose of the vaccine, HI antibody titers 1:40 or more in the younger age group occurred in 92.6% of patients (95% CI 83.7 to 97.6) for A (H1N1), 100% (94.7; 100) for A (H3N2), and 20.6% (11.7; 32.1) for the B strain. In the older age group, titers of 1:40 or more developed in 99.2% (95.4; 100) for A (H1N1), 100% (97; 100) for A (H3N2), and 58.3% (49; 67.3) for the B strain.[30823]
Children and Adolescents 3 to 17 years
A randomized, controlled, double-blind study assessed the immune response to the Fluarix quadrivalent vaccine (n = 791) compared to 2 different formulations of the trivalent Fluarix vaccine, TIV-1 (n = 818) and TIV-2 (n = 801). The quadrivalent vaccine demonstrated non-inferiority to the trivalent formulations at evaluation 28 days after the last vaccination. Seroconversion was defined as a pre-vaccination HI titer of less than 1:10 with a post-vaccination titer of 1:40 or more or at least a 4-fold increase in serum HI titer over baseline to 1:40 or more. Seroconversion occurred in the following percentages of patients for each strain: A/California/7/2009 (H1N1) 91.4% quadrivalent vs. 89.9 to 91.6% trivalent; A/Victoria/210/2009 (H2N2) 72.3% vs. 70.7 to 71.9%; B/Brisbane/60/2008 (Victoria lineage) 70% vs. 29.6 to 68.5%; B/Brisbane/3/2007 (Yamagata lineage) 72.5% vs. 37 to 70.8%. The additional B virus strain in the quadrivalent vaccine did not demonstrate immune interference with the other strains present in the vaccine.[52652]
The efficacy of Afluria in 206 healthy elderly patients (mean age of 72 years, range 65 to 93 years) was assessed by determining the percentage of patients with seroconversion, which was defined as a 4-fold increase in post-vaccination hemagglutination-inhibiting antibody titer if the pre-vaccination titer was at least 1:10 or an increase in titer to at least 1:40 if the pre-vaccination titer was less than 1:10. The mean seroconversion rate ranged from 34% to 45.6% for the 3 vaccine strains. After vaccination, 77.7 to 99.5% had a hemagglutination-inhibiting antibody titer of at least 1:40.[61129] The efficacy of the influenza virus vaccine among older patients was also examined in another study. Receipt of a single dose of the 2003/2004 influenza vaccine to patients either older or younger than 60 years on hemodialysis led to a significant increase from baseline in the percentage of patients with an antibody titer for each of the 3 vaccine strains of at least 1:40, which is considered protective against infection. Fewer older patients obtained a protective antibody titer. For example, 1 month after the dose, 94.7% of 19 patients 60 years of age or younger and 66.7% of 39 patients older than 60 years of age had protective antibody titers against the H1N1 component. The effect of a second dose given a month after the initial dose was examined. The percentage of patients with protective antibody titers did not significantly increase after a second dose. Further, geometric mean titers did not significantly increase after the second dose in either the younger or older patients. The strains in the 2003/2004 influenza vaccine were B/Hong Kong/330/2001(B), A/New Caledonia/20/99 (A/H1N1), and A/Panama/2007/99 (A/H3N2).[33455] In contrast to results obtained after a second dose, more adults at least 65 years of age seroconverted after receipt of Fluzone High-Dose (180 mcg influenza virus hemagglutinin) as compared with receipt of Fluzone (45 mcg influenza virus hemagglutinin). Among the Fluzone High-Dose recipients, 41.8% to 69.1% seroconverted as compared with 23.1% to 50.7% of Fluzone recipients. In another study, administering Fluzone High-Dose to patients 65 years of age and older (n = 15,892) was found to be statistically superior to Fluzone (n = 15,911) in reducing the number of laboratory confirmed influenza cases [1.43% (n = 227) vs. 1.89% (n = 300); 95% CI, 24.2 (9.7; 36.5)].[51849]
Influenza virus vaccine is compatible with breast-feeding. The Advisory Committee on Immunization Practices (ACIP) and the American Academy of Pediatrics (AAP) state inactivated virus vaccines pose no risk for breast-feeding individuals or their children. Additionally, breast-feeding does not adversely affect immunization; limited data suggest breast-feeding may enhance the immune response to certain vaccine antigens. There are no available data regarding the presence of the influenza virus vaccine in human milk, its effects on the breastfed child, or its effects on milk production. No adverse effects have been reported in children potentially exposed to influenza virus vaccine through breast milk.[30823] [41448] [41685] [47301] [52415] [52915] [63436] [65107] [70365] [71393]
No adequate and well-controlled studies have been conducted in pregnant individuals. Based on available data from pregnancy registries of Flucelvax and Fluarix administered during pregnancy, there was no evidence of vaccine-associated risk of major birth defects or miscarriage.[41685] [52415] Data from a post-licensure observational, retrospective safety surveillance study showed no evidence of a vaccine-associated increase in the risk of birth defects and miscarriages when Flublok quadrivalent is administered during pregnancy.[52915] Data from a Pregnancy Exposure Registry in the U.S. looked at individuals vaccinated with Afluria quadrivalent vaccine during the influenza season 2017 to 2018 through 2020 to 2021. Of 483 pregnancies, 477 resulted in live births with 485 infants born. There were 2 stillbirths, neither with major birth defects (1 patient was vaccinated in the first trimester and 1 patient was vaccinated during the second trimester). There were 160 patients vaccinated before 20 weeks gestation, in these patients there were 4 spontaneous abortions (2.5%). Among the 171 patients vaccinated in the first trimester, there were 2 major birth defects (1.2%). In the 201 patients vaccinated in the second trimester, there were 2 major birth defects (1%). The data generated from this registry demonstrates rates of miscarriage and major birth defects that are consistent with the estimated background rates.[61129] During animal studies, no evidence of impaired fertility or fetal harm was noted with influenza vaccines. Pregnancy may increase the risk of serious medical complications from influenza. Therefore, the Advisory Committee on Immunization Practices (ACIP) recommends that all individuals who are or will be pregnant (in any trimester) during the influenza season be routinely vaccinated with an inactivated influenza vaccine (vs. live-attenuated influenza vaccine).[41685] [63436] The American College of Obstetricians and Gynecologist (ACOG) committee also recommends pregnant individuals receive the inactivated or recombinant influenza vaccine as soon as it becomes available. Ideally, the influenza vaccine should be given by the end of October in the United States, but vaccination during flu season can occur at anytime. It is safe and effective to administer other non-virus containing or inactive vaccines (Tdap, RSV, or Covid-19 vaccine) during the same visit.[70419] In addition to benefits to the pregnant person, influenza vaccine administration during pregnancy appears to help protect newborns and infants. Fewer cases of laboratory-confirmed influenza occurred during the first 6 months of life among infants of the 159 mothers who received the inactivated influenza vaccine (6 cases) as compared with infants of 157 mothers who received the pneumococcal polysaccharide vaccine (16 cases). Some manufacturers have established pregnancy registries to monitor pregnancy outcomes and newborn health after vaccination. Individuals who receive these vaccines during pregnancy are encouraged to enroll in these registries. Individuals who receive Flublok during pregnancy are encouraged to call 1-800-822-2463 or complete information online at https://www.sanofipasteurpregnancyregistry.com.[30823] [41448] [41685] [47301] [52415] [52915] [71393]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.