ThisiscontentfromElsevier'sDrugInformation
Liraglutide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
0.6 mg subcutaneously once daily for 1 week, then 1.2 mg subcutaneously once daily, initially. May increase the dose after at least 1 week to 1.8 mg subcutaneously once daily if additional glycemic control is needed. The 0.6 mg dose is a starting dose intended to reduce gastrointestinal symptoms during initial titration and is not effective for glycemic control.[38653]
0.6 mg subcutaneously once daily, initially. May increase the dose after at least 1 week to 1.2 mg subcutaneously once daily and then after at least 1 week to 1.8 mg subcutaneously once daily if additional glycemic control is needed.[38653]
0.6 mg subcutaneously once daily for 1 week, then 1.2 mg subcutaneously once daily, initially. May increase the dose after at least 1 week to 1.8 mg subcutaneously once daily if additional glycemic control is needed. The 0.6 mg dose is a starting dose intended to reduce gastrointestinal symptoms during initial titration and is not effective for glycemic control.[38653]
NOTE: Liraglutide is indicated in adults with a body weight more than 60 kg and obesity or overweight in the presence of at least 1 weight-related comorbid condition and pediatric individuals with a body weight more than 60 kg and obesity.[58673]
0.6 mg subcutaneously once daily for 1 week, then increase the dose by 0.6 mg/week to 3 mg subcutaneously once daily. Consider delaying dose escalation for 1 additional week if a dose increase is not tolerated. Discontinue use if the 3 mg dose is not tolerated; efficacy has not been established at lower doses. If weight loss is not at least 4% of baseline weight after 16 weeks, discontinue therapy.[58673] Pharmacotherapy should be offered as chronic treatment along with lifestyle modifications to individuals affected by obesity when the potential benefits outweigh the risks. Short-term pharmacotherapy has not been shown to produce longer-term health benefits and cannot be generally recommended.[62881]
0.6 mg subcutaneously once daily for 1 week, then increase the dose by 0.6 mg/week to 3 mg subcutaneously once daily. May lower dose to previous level if a dose increase is not tolerated during dose escalation; dose escalation may take up to 8 weeks. Discontinue use if the 2.4 mg dose is not tolerated; efficacy has not been established at lower doses. If weight loss is not at least 1% of baseline BMI after 12 weeks on the maintenance dose, discontinue therapy.[58673] [71238]
0.3 mg subcutaneously once daily for 1 week, then increase the dose by 0.3 mg/week to 1.2 mg subcutaneously once daily, and then increase the dose by 0.6 mg/week to 3 mg subcutaneously once daily. In a small trial, pediatric subjects (age 7 to 11 years) at Tanner stage 1 with obesity were randomized (2:1) to receive 7 to 13 weeks of treatment with liraglutide (n = 16) or placebo (n = 8). A significant decrease in BMI Z score from baseline to end of treatment (estimated treatment difference: -0.28; p = 0.0062) was reported. Body weight was not significantly decreased and may be due to the short duration of treatment.[64813] [71238]
0.6 mg subcutaneously once daily for 1 week, then 1.2 mg subcutaneously once daily for 1 week, then 1.8 mg subcutaneously once daily as the maintenance dose. In people with a BMI of 27 kg/m2 or greater, increase the dose after at least 1 week on the 1.8 mg daily dose to 3 mg subcutaneously once daily.[64926] [68793] [71760]
Blood glucose goals for adults with type 1 or type 2 diabetes [64926]:
A1C goals for adults with type 1 or type 2 diabetes [64926]:
A1C goals for children and adolescents with type 2 diabetes [64926]:
1.8 mg/day subcutaneously for the treatment of type 2 diabetes mellitus; 3 mg/day subcutaneously for the treatment of obesity.
1.8 mg/day subcutaneously for the treatment of type 2 diabetes mellitus; 3 mg/day subcutaneously for the treatment of obesity.
1.8 mg/day subcutaneously for the treatment of type 2 diabetes mellitus; 3 mg/day subcutaneously for the treatment of obesity.
12 years: 1.8 mg/day subcutaneously for the treatment of type 2 diabetes mellitus; 3 mg/day subcutaneously for the treatment of obesity.
10 to 11 years: 1.8 mg/day for the treatment of type 2 diabetes mellitus; safety and efficacy for the treatment of obesity have not been established; however, doses up to 3 mg/day have been used off-label.
7 to 9 years: Safety and efficacy have not been established; however, doses up to 3 mg/day have been used off-label for the treatment of obesity.
1 to 6 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed. However, use liraglutide with caution in patients with hepatic disease. There is limited experience in patients with mild, moderate, or severe hepatic impairment.[38653][58673] Guidelines recommend that liraglutide be used cautiously in patients with hepatic impairment, and avoided in patients with severe hepatic impairment (i.e., Child-Pugh score greater than 9).[62881]
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed. However, use caution when initiating or increasing doses of liraglutide for type 2 diabetes mellitus (T2DM) or weight loss in patients with renal impairment. There are limited data available regarding the use of liraglutide in patients with end-stage renal disease (renal failure). There have been postmarketing reports of acute kidney injury, renal failure, and worsening of chronic renal failure, which sometimes has required hemodialysis in patients treated with liraglutide or other GLP-1 receptor agonists; in many of these cases, altered renal function has been reversed with supportive treatment and discontinuation of potentially causative agents.[38653][58673] Obesity Clinical Practice Guidelines recommend that liraglutide for weight loss can be used in patients with mild to moderate renal impairment (i.e., CrCl 30 to 79 mL/minute). Liraglutide can be considered in selected patients with end-stage renal disease with a high level of caution.[62881]
† Off-label indication
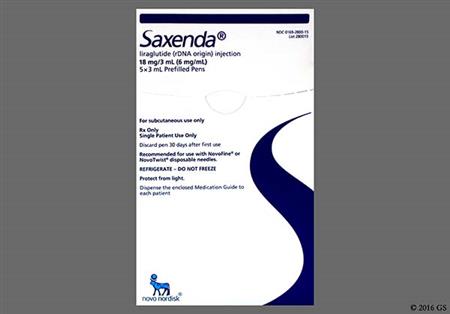
Liraglutide is a synthetic glucagon-like peptide-1 receptor agonist (GLP-1 RA) and belongs to a class of antidiabetic agents called incretin mimetics. Incretins are endogenous compounds that improve glycemic control once released into the circulation via the gut. Liraglutide subcutaneous injection (Victoza) is used as an adjunct to diet and exercise to improve glycemic control in adult and pediatric patients 10 years of age and older with type 2 diabetes mellitus (T2DM). It is also used to reduce the risk of non-fatal cardiovascular (CV) events and CV mortality in adults with T2DM who also have CV disease.[38653][61921] Liraglutide monotherapy reduces A1C by an average of 0.84% to 1.14%. The addition of liraglutide as add-on therapy to other antidiabetic agents has resulted in statistically significant improvements in A1C and fasting plasma glucose. As with other agents in this class, liraglutide has a boxed warning regarding rodent C-cell tumor findings and the uncertain relevance to humans.[38653][38654][38655][38656][38657][38658][40249] First-line T2DM therapy depends on comorbidities, patient-centered treatment factors, and management needs. In adults with T2DM and established atherosclerotic cardiovascular disease (ASCVD) or indicators of high ASCVD risk, a GLP-1 RA with proven CV benefit (e.g., liraglutide, semaglutide, or dulaglutide) should be initiated as a first-line therapy independent of A1C goal or other antihyperglycemic treatments, including metformin. Alternatively, a sodium-glucose co-transporter 2 inhibitor (SGLT2 inhibitor) with proven CV benefit (e.g., canagliflozin, empagliflozin), may be used to reduce the risk of major cardiovascular events (MACE) or CV death in persons with T2DM and established ASCVD. GLP-1 RAs improve CV outcomes, as well as secondary outcomes such as progression of renal disease, in patients with established CV disease or chronic kidney disease (CKD); these factors make GLP-1 RA therapy an alternative initial treatment option, with or without metformin based on glycemic needs, in T2DM patients with indicators of high-risk or established heart failure (HF) or CKD who cannot tolerate an SGLT2 inhibitor. In patients with T2DM who do not have ASCVD/indicators of high-risk, HF, or CKD and who need to minimize hypoglycemia and/or promote weight loss, GLP-1 RAs, including dual glucose-dependent insulinotropic polypeptide (GIP)/ GLP-1 agonists are generally recommended as a second-line option as add-on to metformin therapy. GLP-1 RAs and dual GIP/ GLP-1 agonists have high glucose-lowering efficacy; evidence suggests that the glucose-lowering effect may be greatest for tirzepatide, followed by semaglutide once weekly, dulaglutide and liraglutide, closely followed by exenatide once weekly, and then exenatide twice daily and lixisenatide. Semaglutide and tirzepatide produce the most weight loss, followed by dulaglutide and liraglutide, and then exenatide and lixisenatide. For patients requiring an injectable medication, GLP-1 RAs and dual GIP/ GLP-1 agonists are preferred to insulin due to similar or even better efficacy in A1C reduction, lower risk of hypoglycemia, and reductions in body weight.[50321][64926][60608] Liraglutide injection (Saxenda) is indicated as an adjunct to lifestyle modifications for weight loss and chronic weight management in adults who are obese (BMI 30 kg/m2 or more) or overweight (BMI 27 kg/m2 in the presence of at least 1 weight related condition, such as hypertension, T2DM, or dyslipidemia) and for pediatric patients 12 years of age and older with a body weight more than 60 kg and an initial BMI corresponding to 30 kg/m2 or greater for adults (obese) by international cut-offs (Cole Criteria).[58673] According to the American Association of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE) Obesity Clinical Practice Guidelines, weight loss medications should be offered as chronic treatment along with lifestyle modifications to patients with obesity when the potential benefits outweigh the risks. Short-term pharmacotherapy has not been shown to produce longer-term health benefits and cannot be generally recommended. A generalized hierarchy for medication preferences that would apply to all overweight patients cannot currently be scientifically justified. Individualized weight loss pharmacotherapy is recommended, based upon factors such as the specific characteristics of each weight loss medication, the presence of weight-related complications, and the medical history of the patient.[62881] Liraglutide was initially FDA approved in 2010.[38653][58673]
For storage information, see the specific product information within the How Supplied section.
Hypoglycemia in adult patients that were able to self-treat for type 2 diabetes occurred in 9.7% of patients taking liraglutide monotherapy, in 7.5% of patients taking liraglutide plus glimepiride, and in 27.4% of patients taking liraglutide in combination with glimepiride and metformin. Hypoglycemia requiring the assistance of another person for treatment occurred in 11 patients treated with liraglutide and in 2 comparator-treated patients. Of these 11 patients treated with liraglutide, 6 patients were concomitantly using metformin and a sulfonylurea, 1 was concomitantly using a sulfonylurea, 2 were concomitantly using metformin (blood glucose values were 65 and 94 mg/dL), and 2 were using liraglutide as monotherapy (1 of these patients was undergoing an intravenous glucose tolerance test, and the other was receiving insulin as treatment during a hospital stay). For these 2 patients on liraglutide monotherapy, the insulin treatment was the likely explanation for the hypoglycemia. In the 26-week open-label trial comparing liraglutide to sitagliptin, the incidence of hypoglycemic events defined as symptoms accompanied by a fingerstick glucose less than 56 mg/dL was comparable among the treatment groups (approximately 5%).[38653] Hypoglycemia (blood glucose less than 54 mg/dL) was reported in 24.2% of pediatric patients with type 2 diabetes receiving liraglutide vs. 10.3% of patients receiving placebo during a 52 week trial period. There was 1 severe episode in the placebo group in an insulin-treated patient. During a clinical trial for weight management in pediatric patients, 15.2% of 125 liraglutide-treated patients had hypoglycemia with a blood glucose less than 70 mg/dL and symptoms compared to 4% of 126 placebo-treated patients. Clinically significant hypoglycemia (blood glucose less than 54 mg/dL) occurred in 1.6% of 125 liraglutide-treated patients and in 0.8% of 126 placebo-treated patients. There were no severe hypoglycemic episodes (an episode requiring the assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions) with liraglutide.[38653] [58673] [64323] Hypoglycemia was reported in 23% of adult patients with type 2 diabetes receiving liraglutide for weight management (Saxenda). In a clinical trial involving adult patients with type 2 diabetes mellitus and overweight or obesity, severe hypoglycemia (defined as requiring the assistance of another person) occurred in 3 (0.7%) of 422 liraglutide-treated patients and in none of the 212 placebo-treated patients. Each of these 3 liraglutide-treated patients was also taking a sulfonylurea. In the same trial, among patients taking a sulfonylurea, documented symptomatic hypoglycemia (defined as documented symptoms of hypoglycemia in combination with a plasma glucose 70 mg/dL or less) occurred in 48 (43.6%) of 110 liraglutide-treated patients and 15 (27.3%) of 55 placebo-treated patients. The doses of sulfonylureas were reduced by 50% at the beginning of the trial per protocol. Among patients not taking a sulfonylurea, documented symptomatic hypoglycemia occurred in 49 (15.7%) of 312 liraglutide-treated patients and 12 (7.6%) of 157 placebo-treated patients. In clinical trials involving patients without type 2 diabetes receiving liraglutide for weight management (Saxenda), there was no systematic capturing or reporting of hypoglycemia, as patients were not provided with blood glucose meters or hypoglycemia diaries. Spontaneously reported symptomatic episodes of unconfirmed hypoglycemia were reported by 46 (1.6%) of 2,962 liraglutide-treated patients and 19 (1.1%) of 1,729 placebo-treated patients. Fasting plasma glucose values obtained at routine clinic visits of 70 mg/dL or less, irrespective of hypoglycemic symptoms, were reported as hypoglycemia in 92 (3.1%) liraglutide-treated patients and 13 (0.8%) placebo-treated patients. The presence of anti-liraglutide antibodies may be associated with a higher incidence of hypoglycemia. In clinical trials, these events were usually classified as mild and resolved while patients continued on treatment. When initiating liraglutide in patients taking insulin secretagogues (such as sulfonylureas), consider reducing the dose of the insulin secretagogue to reduce the risk for hypoglycemia, and monitor blood glucose. In order to decrease the risk of hypoglycemia, the manufacturer of Saxenda (liraglutide for weight management) also recommends reducing the dose of the insulin secretagogue (for example, by one-half) to reduce the risk for hypoglycemia. Conversely, if discontinuing liraglutide in patients with type 2 diabetes, monitor for an increase in blood glucose.[58673]
Gastrointestinal (GI) side effects are among the most common adverse events associated with liraglutide and are sometimes severe. In liraglutide clinical trials, severe GI adverse reactions were reported more frequently among subjects receiving liraglutide for weight maintenance (4.8%) and diabetes (1.2 mg 4.4%, 1.8 mg 4.2%) compared to placebo (1.4% and 1.1%, respectively).[38653] [58673] In the controlled clinical trials of at least 26 weeks duration in subjects with diabetes, gastrointestinal events were the most common category of adverse events among liraglutide-treated antibody-negative subjects (43%, 18%, and 19% of antibody-negative liraglutide-treated, placebo-treated, and active-control-treated subjects, respectively). The most common reasons for withdrawal in the subjects treated with liraglutide for diabetes were nausea (2.8%) and vomiting (1.5%); the comparator group had no subjects withdraw due to nausea and 0.1% due to vomiting. Withdrawal due to gastrointestinal adverse events mostly occurred during the first 2 to 3 months of treatment for diabetes; the percentage of subjects who reported nausea declined over time. In the 52-week monotherapy trial for diabetes, nausea and vomiting occurred at a high rate overall in the liraglutide treated adult subjects (28.4% and 10.9%, respectively) compared to glimepiride-treated subjects (8.5% and 3.6%, respectively); nausea and vomiting were among the most common adverse events associated with liraglutide.[38656] In a 52-week trial for diabetes, nausea (28.8% vs. 13.2% placebo), vomiting (25.8% vs. 8.8% placebo), and diarrhea (22.7% vs. 16.2% placebo) were the most commonly reported adverse events in pediatric patients ages 10 to 17 treated with liraglutide.[64323] Gastrointestinal events from liraglutide in subjects with diabetes were dose-dependent and also included diarrhea (17.1% vs. 8.9% glimepiride) and constipation (9.9% vs. 4.8% glimepiride).[38656] In 26-week combination therapy trials (i.e., liraglutide used with metformin, glimepiride, metformin plus rosiglitazone, and metformin plus glimepiride) in subjects with diabetes, nausea occurred in 7.5% to 34.6% of subjects and vomiting occurred in 6.6% to 12.4% of subjects. Other gastrointestinal adverse events that were seen during the 26-week combination therapy trials in subjects with diabetes were dyspepsia, anorexia, and decreased appetite.[38655] [38657] [38658] [38654] In a 26-week trial comparing liraglutide and sitagliptin in subjects with diabetes, both in combination with metformin, the following gastrointestinal events were reported at a higher incidence with liraglutide compared to sitagliptin: nausea (23.9% vs. 4.6%), diarrhea (9.3% vs. 4.6%), and vomiting (8.7% vs. 4.1%). Severe GI adverse reactions including ileus, GI obstruction, and severe constipation including fecal impaction were reported during postmarketing experience.[38653] [58673] In the clinical trials of liraglutide for weight management, approximately 68% of adult subjects receiving liraglutide and 39% of subjects receiving placebo reported gastrointestinal disorders; the most frequently reported was nausea (39% vs. 14% placebo). Other common adverse reactions that occurred at a higher incidence among adult subjects receiving liraglutide for weight management included diarrhea (20.9%), constipation (19.4%), vomiting (15.7%), dyspepsia (9.6%), xerostomia (2.3%), gastritis, gastroesophageal reflux disease (4.7%), flatulence (4%), eructation (4.5%), abdominal pain (5.4%), upper abdominal pain (5.1%), abdominal distension (4.5%), and anorexia (10%). In adult subjects receiving liraglutide for weight management, most gastrointestinal events were mild or moderate and did not lead to discontinuation of therapy; 6.2% of subjects receiving liraglutide discontinued treatment as a result of gastrointestinal adverse reactions compared to 0.8% of subjects receiving placebo. The most common adverse reactions leading to discontinuation were nausea (2.9%), vomiting (1.7%), and diarrhea (1.4%). The percentage of adult subjects reporting nausea declined as treatment continued. In a pediatric clinical trial for weight management, nausea (42.4%), vomiting (34.3%), diarrhea (22.4%), gastroenteritis (12.8%), abdominal discomfort (4.8%), constipation (4.8%), dyspepsia (4%), and flatulence (3.2%) were reported in liraglutide-treated subjects. Of the pediatric patients receiving liraglutide for weight management, 8% discontinued treatment as a result of gastrointestinal adverse reactions compared to 0% of subjects receiving placebo. The most common adverse reactions leading to discontinuation were vomiting (4.8%) and nausea (3.2%). There have been reports of gastrointestinal adverse reactions, such as nausea, vomiting, and diarrhea, associated with dehydration, volume depletion, and renal impairment in adult subjects receiving liraglutide for weight management. Dysgeusia was mainly reported within the first 12 weeks of treatment with liraglutide for weight management and was often co-reported with gastrointestinal events such as nausea, vomiting, and diarrhea. Liraglutide is not recommended in people with gastroparesis.[38653][58673]
Hepatic adverse reactions and adverse reactions of the gallbladder have been reported with liraglutide. Elevated hepatic enzymes were reported in patients treated with liraglutide for weight management. Increases in alanine aminotransferase (ALT) 10 times or more the upper limit of normal (ULN) were observed in 5 (0.15%) liraglutide-treated patients (two of whom had ALT more than 20- and 40-times the ULN) compared with 1 (0.05%) placebo-treated patient during the liraglutide clinical trials. Clinical evaluation to exclude alternative causes of ALT and aspartate aminotransferase (AST) increases was not done in most cases; therefore, the relationship to liraglutide is uncertain. Some increases in ALT and AST were associated with other confounding factors (such as gallstones). In 5 clinical trials of at least 26 weeks duration, mildly elevated serum bilirubin concentrations (defined as elevations to no more than twice the upper limit of the reference range) occurred in 4% of liraglutide-treated patients, 2.1% of placebo-treated patients and 3.5% of active-comparator-treated patients; other hepatic function tests were not found to be abnormal. During postmarketing experience with liraglutide elevated hepatic enzymes, hyperbilirubinemia, cholestasis, and hepatitis have been reported. In clinical trials of patients receiving liraglutide for weight management (doses up to 3 mg), 2.2% of patients receiving liraglutide reported adverse events of cholelithiasis versus 0.8% of patients receiving placebo. The incidence of cholecystitis was 0.8% in liraglutide-treated patients versus 0.4% in placebo-treated patients. The majority of liraglutide-treated patients with adverse events of cholelithiasis and cholecystitis required cholecystectomy. Substantial or rapid weight loss can increase the risk of cholelithiasis; however, the incidence of acute gallbladder disease was greater in liraglutide-treated patients than in placebo-treated patients even after accounting for the degree of weight loss. In clinical trials of liraglutide for diabetes management, the incidence of cholelithiasis (0.3%) and cholecystitis (0.2%) was the same in both liraglutide-treated and placebo-treated patients. In the LEADER trial, 3.1% of liraglutide-treated patients versus 1.9% of placebo-treated patients reported an acute gallbladder disease event, such as cholelithiasis or cholecystitis. The majority of events required hospitalization or cholecystectomy.[38653] [61921] Patients should be informed that substantial or rapid weight loss can increase the risk of cholelithiasis. Cholelithiasis may also occur in the absence of substantial or rapid weight loss. Patients should be instructed to contact their physician if cholelithiasis is suspected for appropriate clinical follow-up. If cholelithiasis is suspected, gallbladder studies and appropriate clinical follow-up are indicated.[38653] [58673]
Acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in people treated with GLP-1 receptor agonists and during postmarketing surveillance. In clinical trials in subjects receiving liraglutide for diabetes, there were 13 cases (9 acute and 4 chronic) of pancreatitis in subjects treated with liraglutide and 1 case among comparator-treated subjects (2.7 vs. 0.5 cases per 1,000 patient-years). In 1 case of a subject treated with liraglutide for diabetes, the subjects experienced pancreatitis with necrosis and eventually died; clinical causality could not be established. In some of these subjects other risk factors for pancreatitis were present, such as cholelithiasis or alcoholism. Conclusive data to establish a risk of pancreatitis with liraglutide is lacking.[38653] In clinical trials of adult subjects receiving liraglutide for weight management, acute pancreatitis was confirmed by adjudication in 9 (0.3%) of 3,291 subjects compared to 2 (0.1%) of 1,843 subjects receiving placebo. In addition, there were 2 cases of acute pancreatitis in subjects receiving liraglutide who prematurely withdrew from these trials, occurring 74 and 124 days after the last dose, 1 case in a liraglutide-treated subjects during an off-treatment follow-up period within 2 weeks of discontinuing liraglutide, and 1 case that occurred in a subject who completed treatment and was off-treatment for 106 days. In a pediatric clinical trial for weight management, pancreatitis was reported in 1 (0.8%) of the 125 subjects receiving liraglutide; treatment was discontinued in this subject. Additionally, increased lipase was reported in 3.2% of subjects. In adult subjects receiving liraglutide for weight management, 2.1% had a lipase value at anytime during treatment of 3 times or more the upper limit of normal (ULN) compared with 1% of placebo-treated subjects. Hyperamylasemia (defined as an amylase value at anytime in the trial of 3 times or more the ULN) was reported in 0.1% of subjects receiving liraglutide versus 0.1% of subjects receiving placebo. In a placebo-controlled trial in renal impairment subjects receiving liraglutide for diabetes management, a mean increase of 33% for lipase and 15% for amylase from baseline was observed for liraglutide-treated subjectss while placebo-treated subjects had a mean decrease in lipase of 3% and a mean increase in amylase of 1%. In the LEADER trial, serum lipase and amylase were routinely measured. Among liraglutide-treated subjects, 7.9% had a lipase value at any time during treatment of greater than or equal to 3 times the ULN compared with 4.5% of placebo-treated subjects, and 1% of liraglutide-treated subjects had an amylase value at any time during treatment of greater than or equal to 3 times the ULN versus 0.7% of placebo-treated subjects.[61921] The clinical significance of elevations in lipase or amylase with liraglutide is unknown in the absence of other signs and symptoms of pancreatitis.[38653] [58673] The FDA has evaluated unpublished findings that suggest an increased risk of pancreatitis and pre-cancerous cellular changes called pancreatic duct metaplasia in subjects treated with incretin mimetics. These findings were based on examination of a small number of pancreatic tissue specimens taken from subjects after they died from unspecified causes.[53573] The FDA and the EMA have stated that after review, the current data do not support an increased risk of pancreatitis and pancreatic cancer in subjects receiving incretin mimetics. The agencies have not reached any new conclusions about safety risks of the incretin mimetics, although they have expressed that the totality of the data that have been reviewed provides reassurance. Pancreatitis will continue to be a risk associated with incretin mimetics until more data are available; recommendations will be communicated once the review is complete.[56778] After initiation of liraglutide, observe individuals carefully for signs and symptoms of pancreatitis (including persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by vomiting). If pancreatitis is suspected, discontinue liraglutide and initiate appropriate management.[38653] [58673]
In adult patients receiving liraglutide for weight management, mean increases in resting heart rate of 2 to 3 beats per minute (bpm) were observed during routine clinical monitoring. More patients treated with liraglutide, compared with placebo, had changes from baseline at 2 consecutive visits of more than 10 bpm (34% versus 19%, respectively) and 20 bpm (5% versus 2%, respectively). In 6% of patients receiving liraglutide, at least 1 resting heart rate greater than 100 bpm was recorded compared with 4% of placebo-treated patients; this occurred at 2 consecutive study visits for 0.9% of liraglutide-treated patients and 0.3% of patients receiving placebo. Sinus tachycardia was reported in 0.6% of patients receiving liraglutide and in 0.1% of patients receiving placebo. In a clinical pharmacology trial that monitored heart rate continuously for 24 hours, liraglutide treatment was associated with a heart rate that was 4 to 9 bpm higher than that observed with placebo; the clinical significance is unclear, especially for patients with cardiac and cerebrovascular disease as a result of limited exposure in these patients in clinical trials. In a pediatric clinical trial for weight management, mean increases from baseline in resting heart rate of 3 to 7 bpm were observed in liraglutide-treated patients. In clinical trials, 11 (0.3%) of 3,384 liraglutide-treated adult patients compared with none of the 1,941 placebo-treated patients had a cardiac conduction disorder, reported as first degree atrioventricular block (AV block), right bundle-branch block, or left bundle-branch block. Adverse reactions related to hypotension (that is, reports of hypotension, orthostatic hypotension, circulatory collapse, and decreased blood pressure) were reported more frequently with liraglutide (1.1%) compared with placebo (0.5%). Systolic blood pressure decreases to less than 80 mmHg were observed in 4 (0.1%) liraglutide-treated patients compared with no placebo-treated patients. One patient receiving liraglutide had hypotension associated with gastrointestinal adverse reactions and renal failure. In addition, hypotension and palpitations have been associated with anaphylactic reactions in patients receiving liraglutide. Heart rate should be monitored at regular intervals consistent with usual clinical practice. Patients receiving liraglutide should inform health care providers of palpitations or feelings of a racing heartbeat while at rest. For patients who experience a sustained increase in resting heart rate, discontinue treatment with liraglutide.[58673]
Anti-liraglutide antibodies were detected in 42 (2.8%) of 1,505 adult patients receiving liraglutide for weight management. Antibodies that had a neutralizing effect on liraglutide in an in vitro assay occurred in 18 (1.2%) of 1,505 patients receiving liraglutide for weight loss. In a pediatric trial, anti-liraglutide antibodies were detected in 14 (12%) of 117 patients receiving liraglutide for weight management; 5 patients (4.3%) had persistent antibodies as defined by more than 2 antibody visits at least 16 weeks apart. Two patients (1.7%) remained positive throughout the follow-up period, 1 patient (0.9%) had antibodies cross-reactive to native GLP-1, and no patients had neutralizing antibodies.[58673] Anti-liraglutide antibodies were detected in 102 (9%) of 1,104 adult patients with type 2 diabetes mellitus receiving liraglutide during clinical trials. Antibodies that cross-reacted with native GLP-1 were detected in 56 (5%) of the 102 patients that developed anti-liraglutide antibodies. The cross-reacting antibodies were not tested for neutralizing effect, and their effect against native GLP-1 is unknown. In vitro, antibodies with a neutralizing effect on liraglutide were seen in 12 (1%) of patients. There was no identified clinically significant effect of anti-liraglutide antibodies on effectiveness of liraglutide.[38653] Infection was the most common adverse event in patients with diabetes who developed anti-liraglutide antibodies (40% compared to 36%, 34%, and 35% of antibody-negative liraglutide-treated, placebo-treated, and active-control-treated patients, respectively). The specific infections which occurred with greater frequency among liraglutide-treated antibody-positive patients were primarily nonserious upper respiratory tract infections (11% antibody-positive patients and among 7%, 7%, and 5% of antibody-negative liraglutide-treated, placebo-treated, and active-control-treated patients, respectively). Among liraglutide-treated antibody-negative patients with diabetes, the most common category of adverse events was that of gastrointestinal (GI) events, which occurred in 43%, 18%, and 19% of antibody-negative liraglutide-treated, placebo-treated, and active-control-treated patients, respectively. When comparing mean A1C of all antibody-positive and antibody-negative patients, the results indicate that antibody formation was not associated with reduced efficacy of liraglutide; however, the 3 patients with the highest titers of anti-liraglutide antibodies had no reduction in A1C with liraglutide treatment. In the LEADER trial, anti-liraglutide antibodies were detected in 11 out of the 1,247 (0.9%) liraglutide-treated patients with antibody measurements. Of the 11 liraglutide-treated patients who developed anti-liraglutide antibodies, none were observed to develop neutralizing antibodies to liraglutide, and 5 patients (0.4%) developed cross-reacting antibodies against native GLP-1.[38653] [61921] In clinical trials of liraglutide in patients with diabetes, events from an aggregate of adverse events potentially related to immunogenicity (e.g., urticaria, angioedema) occurred among 0.8% of the entire cohort of liraglutide-treated patients and among 0.4% of comparator-treated patients. About one-half of the events in this composite for liraglutide-treated patients were reported as urticaria. It should be noted that patients with anti-liraglutide antibodies were not more likely to develop this type of adverse reaction compared to patients who did not develop anti-liraglutide antibodies. Postmarketing reports of serious hypersensitivity reactions, including anaphylactoid reactions, rash, pruritus, and angioedema have been reported in patients receiving liraglutide for diabetes.[38653] Urticaria was reported in 0.7% of patients receiving liraglutide for weight loss. In a pediatric clinical trial for weight management, rash was reported in 3.2% of patients receiving liraglutide. Asthma, bronchial hyperreactivity, bronchospasm, oropharyngeal swelling, facial swelling, pharyngeal edema, and type IV hypersensitivity reactions have been reported in patients treated with liraglutide in clinical trials. Cases of anaphylactic reactions with additional symptoms such as hypotension, palpitations, dyspnea, and edema have been reported with marketed use of liraglutide.[58673]
In premarketing trials of at least 26 weeks duration in patients with diabetes, the incidence of injection site reaction (e.g., injection site rash, erythema) in patients treated with liraglutide was approximately 2%; withdrawal rates due to injection site reactions were less than 0.2% in liraglutide-treated patients.[38653] In adult patients receiving liraglutide for weight management, injection site erythema (2.5%) and injection site reaction (2.5% to 13.9%) were reported. The most common reactions, each reported by 1% to 2.5% of liraglutide-treated patients and more commonly than by placebo-treated patients, included erythema, pruritus, and rash at the injection site. Injection site reaction was the cause for discontinuation of treatment in 0.6% of liraglutide-treated patients and 0.5% of placebo-treated patients. In a pediatric clinical trial for weight management, pain in extremity (4%) and injection site pain (3.2%) were reported in patients receiving liraglutide. Presence of antibodies may be associated with a higher incidence of injection site reactions. In clinical trials, these events were usually classified as mild and resolved while patients continued on treatment.[58673]
In the controlled clinical trials of at least 26 weeks duration in patients with diabetes, infection was the most common adverse event in patients who developed anti-liraglutide antibodies (40% compared to 36%, 34% and 35% of antibody-negative liraglutide-treated, placebo-treated and active-control-treated patients, respectively); the most common infection in these patients was non-serious upper respiratory infections. In the entire cohort of patients receiving liraglutide for weight management, influenza (7.4% vs. 3.6% glimepiride), sinusitis (5.6% vs. 6% glimepiride), and nasopharyngitis (5.2% vs. 5.2% glimepiride) were reported. Urinary tract infection was also reported in 4.3% to 6% of patients taking liraglutide.[38653] [58673] In patients receiving liraglutide for weight management, gastroenteritis (4.7%) and viral gastroenteritis (2.8%) were reported.[58673]
Other notable adverse events that occurred in subjects with diabetes receiving liraglutide were headache (9.1% vs. 9.3% glimepiride), dizziness (5.8% vs. 5.2% glimepiride), back pain (5% vs. 4.4% glimepiride), and hypertension (3% vs. 6% glimepiride).[38653] In a 52 week trial for diabetes, headache (21.2% vs. 19.1% placebo) and dizziness (12.1% vs. 2.9% placebo) were reported in pediatric patients (10 to 17 years) treated with liraglutide.[64323] In subjects receiving liraglutide for weight management, asthenia (2.1%), fatigue (7.5%), malaise, and dizziness (6%) were mainly reported within the first 12 weeks of treatment and were often co-reported with gastrointestinal events such as nausea, vomiting, and diarrhea. Headache was reported in 13.6% of subjects receiving liraglutide for weight management during clinical trials and during the postmarketing experience. In a pediatric clinical trial for weight management, dizziness (10.4%) and fatigue (4.8%) were reported in subjects receiving liraglutide.[58673]
New primary malignancy has been reported in patients receiving liraglutide; however, causality has not been established.[38653] [58673] In clinical trials of patients receiving liraglutide for diabetes mellitus, there were 7 reported cases of papillary thyroid carcinoma in liraglutide-treated patients; there was 1 case in patients treated with placebo (1.5 vs 0.5 cases per 1,000 patient-years). Most were less than 1 cm in greatest diameter and were diagnosed in surgical pathology specimens after thyroidectomy prompted by findings on protocol specified screening with serum calcitonin or thyroid ultrasound. In a pooled analysis of clinical trials, the incidence rate (per 1,000 patient-years) for new primary malignancy was 10.9 for liraglutide, 6.3 for placebo, and 7.2 for active comparator. No particular cancer cell type predominated after excluding papillary thyroid carcinoma events. Seven malignant neoplasm events were reported beyond 1 year of exposure to study medication; 6 events among liraglutide-treated patients (4 colon, 1 prostate and 1 nasopharyngeal), no events with placebo, and 1 event with active comparator (colon). Causality has not been established.[38653] In patients receiving liraglutide for weight management, papillary thyroid carcinoma confirmed by adjudication was reported in 7 (0.2%) of 3,291 patients compared with no cases among 1843 placebo-treated patients. Four of these papillary thyroid carcinomas were less than 1 cm in greatest diameter and four patients were diagnosed in surgical pathology specimens after thyroidectomy prompted by findings identified prior to treatment. Calcitonin, a biological marker of medullary thyroid carcinoma (MTC), was measured throughout the clinical development program. More patients treated with liraglutide in the clinical trials were observed to have high calcitonin values during treatment, compared with placebo. The proportion of patients with calcitonin 2 times or greater the upper limit of normal (ULN) at the end of the trial was 1.2% in liraglutide-treated patients and 0.6% in placebo-treated patients. Calcitonin values greater than 20 ng/L at the end of the trial occurred in 0.5% of liraglutide-treated patients and 0.2% of placebo-treated patients; among patients with pre-treatment serum calcitonin less than 20 ng/L, none had calcitonin elevations to more than 50 ng/L at the end of the trial. In clinical trials of patients receiving liraglutide for weight management, benign colorectal neoplasms (mostly colon adenomas) confirmed by adjudication were reported in 17 (0.5%) of 3,291 patients compared with 4 (0.2%) of 1,843 placebo-treated patients. Two positively adjudicated cases of malignant colorectal carcinoma were reported in liraglutide-treated patients (0.1%) and none in placebo-treated patients. In clinical trials of patients receiving liraglutide for weight management, breast cancer confirmed by adjudication was reported in 14 (0.6%) of 2379 women compared with 3 (0.2%) of 1300 placebo-treated women, including invasive cancer (11 liraglutide- and 2 placebo-treated women) and ductal carcinoma in situ (3 liraglutide- and 1 placebo-treated woman). The majority of cancers were estrogen- and progesterone-receptor positive. There were too few cases to determine whether these cases were related to liraglutide. In addition, there are insufficient data to determine whether liraglutide has an effect on pre-existing breast neoplasia.[58673]
Liraglutide, like other GLP-1 receptor agonists, may be associated with acute kidney injury. There are postmarketing reports of acute kidney injury, acute kidney failure or worsening of chronic renal failure, in some cases requiring hemodialysis, in individuals treated with GLP-1 receptor agonists. A majority of the reported events occurred in individuals who had experienced gastrointestinal adverse reactions leading to dehydration such as nausea, vomiting, and diarrhea. In a pediatric clinical trial for weight management, elevated creatine kinase was reported in 3.2% of subjects receiving liraglutide. Advise individuals of the potential risks of dehydration due to GI adverse reactions and to take precautions to avoid fluid depletion while taking liraglutide. Monitor renal function in individuals reporting adverse reactions to liraglutide that could lead to volume depletion, especially during dosage initiation and escalation of liraglutide. Liraglutide has not been found to be directly nephrotoxic in preclinical or clinical studies.[38653] [58673]
In clinical trials of liraglutide for weight management in adults, 0.3% of patients receiving liraglutide reported suicidal ideation compared to 0.1% of the patients receiving placebo; 1 of the liraglutide-treated patients attempted suicide. In a pediatric clinical trial of liraglutide for weight management, 1 (0.8%) of the 125 patients receiving liraglutide died by suicide. Depression was reported in 4% of pediatric patients receiving liraglutide. Monitor patients receiving liraglutide for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior. Discontinue liraglutide in patients who develop suicidal thoughts or behaviors. Other psychiatric adverse reactions reported in clinical trials of patients receiving liraglutide for the treatment of obesity included insomnia (2.4%) and anxiety (2%).[58673] In January 2024, the FDA announced that they have not found evidence that use of GLP-1 RAs for type 2 diabetes or weight management causes suicidal thoughts or actions. During their preliminary evaluation, they conducted detailed reviews of reports of suicidal thoughts or actions received in the FDA Adverse Event Reporting System (FAERS) and reviews of clinical trials, including large outcome studies and observational studies. However, because of the small number of suicidal thoughts or actions observed in both people using GLP-1 RAs and in the comparative control groups, they cannot definitively rule out that a small risk may exist; therefore, FDA is continuing to look into this issue. Further evaluations include a meta-analysis of clinical trials across all GLP-1 RA products and an analysis of postmarketing data in the Sentinel System; final conclusions and recommendations will be communicated once more information is known.[70130]
In a pediatric clinical trial for weight management, fever (8%), dyslipidemia (4.8%), and cough (4%) were reported in patients receiving liraglutide.[58673]
There have been postmarketing reports of perioperative pulmonary aspiration in patients receiving GLP-1 receptor agonists who underwent elective surgery or procedures requiring general anesthesia or deep sedation. Despite adherence to preoperative fasting guidelines, these patients were found to have residual gastric contents. The available data is insufficient to give recommendations on mitigating the risk of pulmonary aspiration during general anesthesia or deep sedation in patients taking liraglutide, including whether to modify preoperative fasting recommendations or temporarily discontinue liraglutide.[38653]
Alopecia has been reported during post-approval use of liraglutide.[38653] [58673]
Dysesthesia has been reported during post-approval use of liraglutide.[38653] [58673]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Anaphylaxis and angioedema have been reported with GLP-1 receptor agonists. Use liraglutide with caution in people with a history of angioedema or anaphylaxis with a GLP-1 receptor agonist because it is unknown whether such patients will be predisposed to these reactions with liraglutide.[38653][58673]
Liraglutide is contraindicated in people with a personal or family history of medullary thyroid carcinoma (MTC) or in people with multiple endocrine neoplasia syndrome type 2 (MEN 2). Liraglutide has been shown to cause dose-dependent and treatment duration-dependent increase in the incidence of thyroid C-cell tumors (adenomas and carcinomas) in animal studies. It is unknown whether liraglutide causes thyroid C-cell tumors, including MTC, in humans. It is not known whether monitoring serum calcitonin or performing thyroid ultrasounds will diminish human risk of thyroid C-cell tumors. Liraglutide recipients should be counseled on the risk and symptoms of thyroid tumors (e.g. a mass in the neck, dysphagia, dyspnea or persistent hoarseness). Although routine monitoring of serum calcitonin is of uncertain value during liraglutide treatment, if serum calcitonin is measured and found to be elevated, the individual should be referred to an endocrinologist for further evaluation.[38653] [58673]
Liraglutide is not recommended for people with severe gastroparesis. Liraglutide may slow gastric emptying, consistent with the actions of other GLP-1 receptor agonists, and has been associated with gastrointestinal adverse reactions that are sometimes severe.[38653] [58673]
Use liraglutide with caution in people with renal impairment, especially during treatment initiation and at escalation of doses. There is limited experience with liraglutide use in people with mild, moderate, and severe renal impairment, including end-stage renal disease (renal failure). Monitor renal function in people reporting adverse reactions to liraglutide that could lead to volume depletion. There have been postmarketing reports of acute kidney injury, acute renal failure and worsening of chronic renal failure with liraglutide, which may sometimes require hemodialysis. The majority of the reported events occurred in people who experienced gastrointestinal adverse reactions leading to dehydration such as nausea, vomiting, or diarrhea.[38653] [58673]
Avoid liraglutide products for weight management in people with a history of suicidal attempts or active suicidal ideation; use it with caution in people with a history of depression. Suicidal behavior and ideation have been reported in clinical trials with other weight management products. Monitor recipients of liraglutide for weight management for the emergence or worsening of depression, suicidal thoughts or behaviors, and/or any unusual changes in mood or behavior. Discontinue liraglutide in patients who develop suicidal thoughts or behaviors.[58673] In January 2024, the FDA announced that they have not found evidence that use of GLP-1 RAs for type 2 diabetes or weight management causes suicidal thoughts or actions. During their preliminary evaluation, they conducted detailed reviews of reports of suicidal thoughts or actions received in the FDA Adverse Event Reporting System (FAERS) and reviews of clinical trials, including large outcome studies and observational studies. However, because of the small number of suicidal thoughts or actions observed in both people using GLP-1 RAs and in the comparative control groups, they cannot definitively rule out that a small risk may exist; therefore, FDA is continuing to look into this issue. Further evaluations include a meta-analysis of clinical trials across all GLP-1 RA products and an analysis of postmarketing data in the Sentinel System; final conclusions and recommendations will be communicated once more information is known.[70130]
Liraglutide should be used cautiously in those with mild (Child-Pugh class A), moderate (Child-Pugh class B) or severe (Child-Pugh class C) hepatic impairment because there is limited experience in these patients.[38653] [58673]
Use liraglutide with caution in people with a history of pancreatitis. After initiation of liraglutide, observe individuals carefully for signs and symptoms of pancreatitis (including persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by vomiting). Acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in individuals treated with GLP-1 receptor agonists. If pancreatitis is suspected, discontinue liraglutide and initiate appropriate management.[38653] [58673]
Liraglutide (Saxenda) for the treatment of obesity or weight management should not be used during pregnancy because weight loss offers no potential benefit to a pregnant person and may result in fetal harm due to the potential hazard of maternal weight loss to the fetus.[58673] There are no adequate data or clinical studies of liraglutide (Victoza) for the treatment of type 2 diabetes mellitus during pregnancy. Use liraglutide only if the potential benefit justifies the potential risk to the fetus. Because of the toxicities found in animal studies, it may be prudent to avoid liraglutide until human pregnancy data are available. Rat studies have noted abnormalities and variations in the kidneys, and irregular skeletal ossification effects when liraglutide was given at or above 0.8 times the human systemic exposures, based on the maximum recommended human dose (MRHD) of 1.8 mg/day (determined from AUC). Reduced growth and increased total major abnormalities occurred in rabbits at systemic exposures below human exposure at the MRHD (determined from AUC).[38653] The American College of Obstetricians and Gynecologists (ACOG) and the American Diabetes Association (ADA) continue to recommend human insulin as the standard of care for individuals with diabetes mellitus or gestational diabetes mellitus (GDM) requiring medical therapy; insulin does not cross the placenta.[64926] [62358]
Use liraglutide with caution during breast-feeding. Liraglutide excretion into human milk is unknown; however, because it has a high molecular weight the amount in breast milk is likely to be very low and absorption is unlikely because the medication is most likely destroyed in the infant's gastrointestinal tract.[70364] [70365] Consider the benefits of breast-feeding, the risk of potential infant drug exposure to liraglutide, and the risk of an untreated or inadequately treated condition. In lactating rats, liraglutide was excreted unchanged in milk at concentrations approximately 50% of maternal plasma concentrations; the human relevance of thyroid C-cell tumors observed in mice and rats is unknown.[38653] [58673] If liraglutide is discontinued in an individual with type 2 diabetes mellitus (T2DM) and blood glucose is not controlled on diet and exercise alone, insulin therapy may be considered. Oral hypoglycemics may also be considered. Metformin monotherapy may be appropriate for some patients as available studies indicate low excretion in milk and that maternal use during breast-feeding is not expected to result in side effects to a healthy nursing infant. Some experts recommend using metformin with caution if the patient is breastfeeding a newborn or a premature neonate with reduced renal function.[31407] [31408] [31409] [32459] [70364] Because acarbose has limited systemic absorption, which results in minimal maternal plasma concentrations, clinically significant exposure via breast milk is not expected; therefore, this agent may be an alternative if postprandial glucose control is needed.[46303] Glyburide may be a suitable alternative since it was not detected in the breast milk of lactating women who received single and multiple doses of glyburide.[31568] If any oral hypoglycemics are used during breast-feeding, the nursing infant should be monitored for signs of hypoglycemia, such as increased fussiness or somnolence.[46104]
Liraglutide is an incretin mimetic; specifically, liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist with 97% amino acid sequence homology to endogenous GLP-1 (7-37). GLP-1 (7-37) represents less than 20% of total circulating endogenous GLP-1. Liraglutide binds and activates the GLP-1 receptor.[38653] GLP-1 is an important, gut-derived, glucose homeostasis regulator that is released after the oral ingestion of carbohydrates or fats. In patients with type 2 diabetes, GLP-1 concentrations are decreased in response to an oral glucose load. GLP-1 enhances insulin secretion; it increases glucose-dependent insulin synthesis and in vivo secretion of insulin from pancreatic beta cells in the presence of elevated glucose. In addition to increases in insulin secretion and synthesis, GLP-1 suppresses glucagon secretion, slows gastric emptying, reduces food intake, and promotes beta-cell proliferation.[38658] Liraglutide does not increase insulin secretion or suppress glucagon secretion at normal or low glucose concentrations.
GLP-1 is also a physiological regulator of appetite and caloric intake and the GLP-1 receptor is present in several areas of the brain involved in appetite regulation. Liraglutide acts to reduce body weight through decreased caloric intake; it does not increase 24-hour energy expenditure.[58673]
Revision Date: 10/16/2025, 10:21:21 AMLiraglutide is given via subcutaneous administration. Liraglutide is more than 98% bound to plasma protein. After a single radioactive liraglutide dose was administered to healthy subjects, the major component in plasma was intact liraglutide for the initial 24 hours. The mean apparent volume of distribution after subcutaneous administration of a 0.6 mg and 3 mg dose of liraglutide is approximately 13 L and 20 to 25 L, respectively. The metabolism of liraglutide mirrors that of large proteins without a specific organ as a major route of elimination. After a radioactive liraglutide dose, intact liraglutide was not detected in urine or feces; only a minor part of the administered dose was excreted as metabolites in the urine (6%) or feces (5%). The mean apparent clearance after subcutaneous injection of a single dose of liraglutide is approximately 0.9 to 1.4 L/hour. Liraglutide is resistant to dipeptidyl peptidase-4 (DDP-4), the endogenous enzyme responsible for the degradation of GLP-1; this allows for a long half-life (13 hours) and once daily dosing.[38653][58673]
Affected cytochrome P450 (CYP450) enzymes and drug transporters: None
The mean volume of distribution after IV administration is 0.07 L/kg.[38653][58673]
After subcutaneous injection, liraglutide binds to albumin at the injection site, and after that is released slowly into circulation. Peak plasma concentrations are achieved in roughly 8 to 12 hours; after a 0.6 mg subcutaneous dose, mean peak concentration was 35 ng/mL and total area under the curve (AUC) was 960 ng x hour/mL. Liraglutide Cmax and AUC increased proportionally over the therapeutic dose range of 0.6 to 1.8 mg. At a dose of 1.8 mg, the average steady-state concentration over 24 hours was approximately 128 ng/mL. In obese patients (BMI 30 to 40 kg/m2), the average steady-state concentration over 24 hours was approximately 116 ng/mL. Similar absorption is achieved with subcutaneous administration of liraglutide in the abdomen, thigh, or arm. The absolute bioavailability of liraglutide after subcutaneous injection is approximately 55%.[38653] [58673]
The pharmacokinetics of a single dose of liraglutide were evaluated in patients with varying degrees of hepatic impairment. Compared to healthy subjects, the AUC in patients with mild (Child-Pugh score 5 to 6) to severe hepatic impairment (Child-Pugh score more than 9) was on average 11%, 14%, and 42% lower, respectively. Liraglutide should be used with caution in patients with hepatic impairment.[38653] [58673]
The pharmacokinetics of a single dose of liraglutide were evaluated in patients with varying degrees of renal impairment. Compared to healthy subjects, the AUC in patients with mild (CrCl 50 to 80 mL/minute), moderate (CrCl 31 to 49 mL/minute), severe renal impairment (CrCl less than 30 mL/minute), and end-stage renal disease (ESRD) requiring dialysis was on average 35%, 19%, 29%, and 30% lower, respectively. Liraglutide should be used with caution in patients with renal impairment.[38653] [58673]
A population pharmacokinetic analysis conducted in 72 pediatric patients (10 to 17 years of age) with type 2 diabetes and a separate pharmacokinetic analysis conducted in 134 pediatric patients (12 to 17 years of age) with obesity found the pharmacokinetic profile of liraglutide to be consistent with that in adults.[38653][58673]
Age had no effect on the pharmacokinetics of liraglutide based on a pharmacokinetic study in healthy elderly subjects (65 to 83 years) and population pharmacokinetic analyses of patients 18 to 80 years of age.[38653]
Based on the results of population pharmacokinetic analyses, females have 25% lower weight-adjusted clearance of liraglutide compared to males. Based on the exposure response data, no dose adjustment is necessary based on gender.[38653]
Race and ethnicity had no effect on the pharmacokinetics of liraglutide based on the results of population pharmacokinetic analyses that included Caucasian, Black, Asian, and Hispanic/Non-Hispanic subjects.[38653]
Body weight significantly affects the pharmacokinetics of liraglutide based on results of population pharmacokinetic analyses conducted in patients 60 to 234 kg. The exposure of liraglutide decreases with an increase in baseline body weight. At a dose of 1.8 mg, the average steady state concentration over 24 hours was approximately 128 ng/mL. In obese patients (BMI 30 to 40 kg/m2), the average steady state concentration over 24 hours was approximately 116 ng/mL. However, in type 2 diabetes patients with a body weight of 40 to 160 kg, daily doses of 1.2 mg and 1.8 mg provided adequate systemic exposures.[38653][58673]
Liraglutide (Saxenda) for the treatment of obesity or weight management should not be used during pregnancy because weight loss offers no potential benefit to a pregnant person and may result in fetal harm due to the potential hazard of maternal weight loss to the fetus.[58673] There are no adequate data or clinical studies of liraglutide (Victoza) for the treatment of type 2 diabetes mellitus during pregnancy. Use liraglutide only if the potential benefit justifies the potential risk to the fetus. Because of the toxicities found in animal studies, it may be prudent to avoid liraglutide until human pregnancy data are available. Rat studies have noted abnormalities and variations in the kidneys, and irregular skeletal ossification effects when liraglutide was given at or above 0.8 times the human systemic exposures, based on the maximum recommended human dose (MRHD) of 1.8 mg/day (determined from AUC). Reduced growth and increased total major abnormalities occurred in rabbits at systemic exposures below human exposure at the MRHD (determined from AUC).[38653] The American College of Obstetricians and Gynecologists (ACOG) and the American Diabetes Association (ADA) continue to recommend human insulin as the standard of care for individuals with diabetes mellitus or gestational diabetes mellitus (GDM) requiring medical therapy; insulin does not cross the placenta.[64926] [62358]
Use liraglutide with caution during breast-feeding. Liraglutide excretion into human milk is unknown; however, because it has a high molecular weight the amount in breast milk is likely to be very low and absorption is unlikely because the medication is most likely destroyed in the infant's gastrointestinal tract.[70364] [70365] Consider the benefits of breast-feeding, the risk of potential infant drug exposure to liraglutide, and the risk of an untreated or inadequately treated condition. In lactating rats, liraglutide was excreted unchanged in milk at concentrations approximately 50% of maternal plasma concentrations; the human relevance of thyroid C-cell tumors observed in mice and rats is unknown.[38653] [58673] If liraglutide is discontinued in an individual with type 2 diabetes mellitus (T2DM) and blood glucose is not controlled on diet and exercise alone, insulin therapy may be considered. Oral hypoglycemics may also be considered. Metformin monotherapy may be appropriate for some patients as available studies indicate low excretion in milk and that maternal use during breast-feeding is not expected to result in side effects to a healthy nursing infant. Some experts recommend using metformin with caution if the patient is breastfeeding a newborn or a premature neonate with reduced renal function.[31407] [31408] [31409] [32459] [70364] Because acarbose has limited systemic absorption, which results in minimal maternal plasma concentrations, clinically significant exposure via breast milk is not expected; therefore, this agent may be an alternative if postprandial glucose control is needed.[46303] Glyburide may be a suitable alternative since it was not detected in the breast milk of lactating women who received single and multiple doses of glyburide.[31568] If any oral hypoglycemics are used during breast-feeding, the nursing infant should be monitored for signs of hypoglycemia, such as increased fussiness or somnolence.[46104]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.