ThisiscontentfromElsevier'sDrugInformation
Semaglutide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
3 mg PO once daily for 30 days (this dosage is not effective for glycemic control), then 7 mg PO once daily. May increase the dose to 14 mg PO once daily after at least 30 days on 7 mg/day if additional glycemic control is needed.[64637]
1.5 mg PO once daily for 30 days (this dosage is not effective for glycemic control), then 4 mg PO once daily. May increase the dose to 9 mg PO once daily after at least 30 days on 4 mg/day if additional glycemic control is needed.[64637]
7 or 14 mg PO once daily, starting up to 7 days after the last injection of 0.5 mg subcutaneously once weekly. There are no oral dose recommendations for people switching from the 0.25 mg, 1 mg, or 2 mg per week subcutaneous dose.[64637]
4 or 9 mg PO once daily, starting up to 7 days after the last injection of 0.5 mg subcutaneously once weekly. There are no oral dose recommendations for people switching from the 0.25 mg, 1 mg, or 2 mg per week subcutaneous dose.[64637]
Do not switch between Rybelsus formulations during the initiation phase (Days 1 to 30). After 30 days of Rybelsus treatment (after the initiation phase), people may switch between Rybelsus formulations. People taking 7 mg PO once daily of the Rybelsus formulation R1 may switch to 4 mg PO once daily of the Rybelsus formulation R2 the day after discontinuing the previous Rybelsus formulation, and vice versa. People taking 14 mg PO once daily of the Rybelsus formulation R1 may switch to 9 mg PO once daily of the Rybelsus formulation R2 the day after discontinuing the previous Rybelsus formulation, and vice versa.[64637]
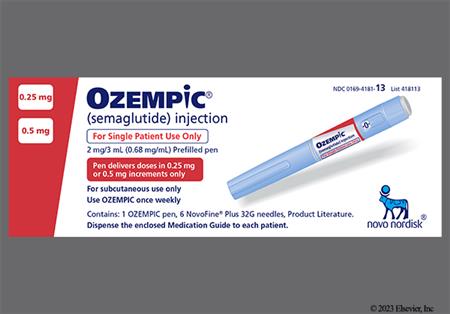
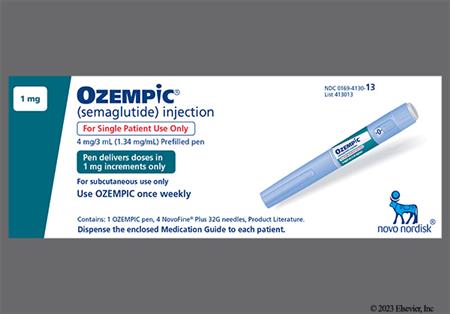
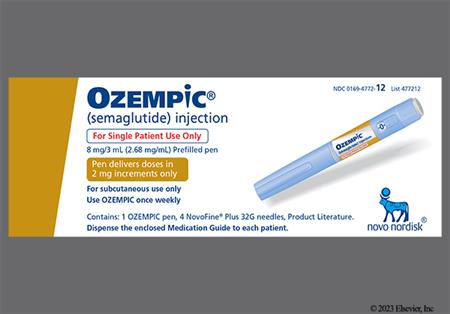
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly, initially. May increase the dose to 1 mg subcutaneously once weekly after 4 weeks on 0.5 mg/week and 2 mg subcutaneously once weekly after 4 weeks on 1 mg/week if additional glycemic control is needed.[62656]
0.5 mg subcutaneously once weekly, starting the day after the last oral dose is the conversion dosage for people currently taking 14 mg PO once daily. No other dosage conversions are available.[64637]
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly, initially. May increase the dose to 1 mg subcutaneously once weekly after 4 weeks on 0.5 mg/week and 2 mg subcutaneously once weekly after 4 weeks on 1 mg/week if additional glycemic control is needed.[62656]
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly for at least 4 weeks, and then 1 mg subcutaneously once weekly.[62656]
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly for 4 weeks, then 1 mg subcutaneously once weekly for 4 weeks, then 1.7 mg subcutaneously once weekly for 4 weeks, and then 2.4 mg (recommended) or 1.7 mg subcutaneously once weekly. Consider delaying dose escalation for 4 weeks if a dose increase is not tolerated. Assess treatment response and tolerability when selecting the maintenance dose.[66713]
NOTE: Semaglutide is indicated in adults and the approved pediatric groups with obesity. It is also approved in overweight adults with at least 1 weight-related comorbid condition.[66713]
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly for 4 weeks, then 1 mg subcutaneously once weekly for 4 weeks, then 1.7 mg subcutaneously once weekly for 4 weeks, and then 1.7 or 2.4 mg (recommended) subcutaneously once weekly. Consider delaying dose escalation for 4 weeks if a dose increase is not tolerated. Assess treatment response and tolerability when selecting the maintenance dose.[66713]
0.25 mg subcutaneously once weekly for 4 weeks, then 0.5 mg subcutaneously once weekly for 4 weeks, then 1 mg subcutaneously once weekly for 4 weeks, then 1.7 mg subcutaneously once weekly for 4 weeks, then 1.7 mg or 2.4 mg (recommended) subcutaneously once weekly. Consider delaying dose escalation for 4 weeks if a dose increase is not tolerated. Assess treatment response and tolerability when selecting the maintenance dose.[66713] [71238]
The indication of MASH is approved under accelerated approval based on improvement of MASH and fibrosis during clinical trials. Continued approval for this indication may be contingent upon the verification and description of clinical benefit in a confirmatory trial.[66713]
0.25 mg subcutaneously once weekly for weeks 1 through 4, then 0.5 mg subcutaneously once weekly for weeks 5 through 8, then 1 mg subcutaneously once weekly for weeks 9 through 12, then 1.7 mg subcutaneously once weekly for weeks 13 through 16. From week 17 and onward, the recommended maintenance dose is 2.4 mg subcutaneously once weekly. Maintenance dose can be decreased to 1.7 mg once weekly if the dose increase is not tolerated. Consider re-escalation to 2.4 mg weekly.[66713]
Blood glucose goals for adults with type 1 or type 2 diabetes [64926]:
A1C goals for adults with type 1 or type 2 diabetes [64926]:
2 mg/week subcutaneously for the treatment of type 2 diabetes mellitus; 2.4 mg/week subcutaneously for the treatment of obesity and noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH); 14 mg/day PO for the treatment of type 2 diabetes mellitus.
2 mg/week subcutaneously for the treatment of type 2 diabetes mellitus; 2.4 mg/week subcutaneously for the treatment of obesity and noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH); 14 mg/day PO for the treatment of type 2 diabetes mellitus.
2.4 mg/week subcutaneously for the treatment of obesity; safety and efficacy have not been established for the treatment of type 2 diabetes mellitus.
12 years: 2.4 mg/week subcutaneously for the treatment of obesity; safety and efficacy have not been established for the treatment of type 2 diabetes mellitus.
1 to 11 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
No dosage adjustments are needed.[62656][64637][66713]
No dosage adjustments are needed; however, use caution in patients with renal impairment or end-stage renal disease (renal failure).[62656][64637][66713]
† Off-label indication








Semaglutide is a synthetic glucagon-like peptide-1 receptor agonist (GLP-1 RA) that belongs to a class of antidiabetic agents called incretin mimetics. Semaglutide subcutaneous injection (Ozempic) and oral tablets (Rybelsus) are indicated as an adjunct to diet and exercise to improve glycemic control in individuals with type 2 diabetes mellitus (T2DM).[62656][64637] Semaglutide subcutaneous injection (Ozempic) is also indicated to reduce the risk of major adverse cardiovascular (CV) events (MACE) in individuals with established CV disease and T2DM and to reduce the risk of sustained estimated glomerular filtration rate (eGFR) decline, end-stage kidney disease, and CV death in individuals with chronic kidney disease (CKD) and T2DM.[62656] Semaglutide subcutaneous injection (Wegovy) is indicated as an adjunct to lifestyle modifications to reduce excess body weight and maintain weight reduction long term in adults and pediatric individuals aged 12 years and older with obesity and adults with overweight in the presence of at least 1 weight-related comorbid condition. Semaglutide subcutaneous injection (Wegovy) is also indicated for noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH) with moderate to advanced liver fibrosis (consistent with stages F2 to F3 fibrosis), and to reduce the risk of MACE in adults with established CV disease and obesity or who are overweight.[66713] First-line T2DM therapy depends on comorbidities, individual-centered treatment factors, and management needs. In adults with T2DM and established atherosclerotic cardiovascular disease (ASCVD) or indicators of high ASCVD risk, a GLP-1 RA with proven CV benefit (e.g., liraglutide, semaglutide, or dulaglutide) should be initiated as a first-line therapy independent of A1C goal or other antihyperglycemic treatments, including metformin. Alternatively, a sodium-glucose co-transporter 2 inhibitor (SGLT2 inhibitor) with proven CV benefit (e.g., canagliflozin, empagliflozin), may be used to reduce the risk of MACE or CV death in persons with T2DM and established ASCVD. GLP-1 RAs improve CV outcomes, as well as secondary outcomes such as progression of renal disease, in individuals with established CV disease or CKD; these factors make GLP-1 RA therapy an alternative initial treatment option, with or without metformin based on glycemic needs, in individuals with T2DM with indicators of high-risk or established heart failure (HF) or CKD who cannot tolerate an SGLT2 inhibitor. In individuals with T2DM who do not have ASCVD/indicators of high-risk, HF, or CKD and who need to minimize hypoglycemia and/or promote weight loss, GLP-1 RAs, including dual glucose-dependent insulinotropic polypeptide (GIP)/ GLP-1 agonists are generally recommended as a second-line option as add-on to metformin therapy. GLP-1 RAs and dual GIP/ GLP-1 agonists have high glucose-lowering efficacy; evidence suggests that the glucose-lowering effect may be greatest for tirzepatide, followed by semaglutide once weekly, dulaglutide and liraglutide, closely followed by exenatide once weekly, and then exenatide twice daily and lixisenatide. Semaglutide and tirzepatide produce the most weight loss, followed by dulaglutide and liraglutide, and then exenatide and lixisenatide.[50321][64926][60608] According to the American Association of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE) Obesity Clinical Practice Guidelines, weight loss medications should be offered as chronic treatment along with lifestyle modifications to individuals with obesity when the potential benefits outweigh the risks. Short-term pharmacotherapy has not been shown to produce longer-term health benefits and cannot be generally recommended. A generalized hierarchy for medication preferences that would apply to all overweight individuals cannot currently be scientifically justified. Individualized weight loss pharmacotherapy is recommended, based upon factors such as the specific characteristics of each weight loss medication, the presence of weight-related complications, and personal medical history.[62881] In a 240-week, randomized, double-blind, placebo-controlled trial, semaglutide (Wegovy) demonstrated improvement of histopathology endpoints including resolution of steatohepatitis and no worsening of liver fibrosis (63%), improvement in liver fibrosis and no worsening of steatohepatitis (37%), and resolution of steatohepatitis and improvement in liver fibrosis (33%) compared to placebo (34%, 22%, and 16%, respectively). Subjects treated with semaglutide (Wegovy) also achieved an average of 10.5% weight loss from baseline (mean baseline body weight 95.4 kg) at week 72 and treatment resulted in an average of 8.5% greater weight loss from baseline compared to placebo. Additionally, there was a trend of greater reductions from baseline in average ALT and AST in subjects in the treatment group compared to placebo.[66713] As with other agents in this class, semaglutide has a boxed warning regarding rodent thyroid C-cell tumor findings and the uncertain relevance to humans.[62656][64637][66713] Semaglutide was FDA-approved in 2017.[62656][64637][66713]
NOTE: In December 2023, the FDA warned about counterfeit semaglutide (Ozempic or Wegovy) products. Wholesalers, retail pharmacies, health care practitioners, and consumers are advised to check the products they have received and not distribute, use, or sell products labeled with lot number NAR0074 and serial number 430834149057. The FDA and Novo Nordisk are testing the seized products and do not yet have information about the drugs' identity, quality, or safety. Analysis found the needles from the samples are counterfeit and therefore, the sterility of the needles cannot be confirmed, which presents an increased risk of infection. Other confirmed counterfeit components within the seized products are the pen label, accompanying health care professional and consumer information, and carton. The FDA is aware of 5 adverse events from this lot, none of which are serious and are consistent with known common adverse reactions to authentic semaglutide. The FDA recommends retail pharmacies only purchase authentic products through authorized distributors and review the photographs and information to confirm the legitimacy of their shipments. Individuals should only obtain semaglutide products with a valid prescription through state-licensed pharmacies and check the product before using for any signs of counterfeiting. Health care professionals and consumers should report adverse events related to the use of this product to FDA's MedWatch Safety Information and Adverse Event Reporting Program. Retailers and consumers may also contact Novo Nordisk customer care at 1-800-727-6500 with questions or concerns.[70063] The FDA has established a "green list" import alert to help stop potentially dangerous GLP-1 RA active pharmaceutical ingredients (APIs) from unverified foreign sources from entering the U.S. market. This is part of the agency's decisive steps to safeguard consumers from illegal GLP-1 RA active ingredients imported from overseas to ensure safety and a secure drug supply chain. To protect people who use compounded versions of GLP-1 RAs, the green list will include GLP-1 APIs from facilities the agency has inspected or evaluated that appear to be in compliance with the FDA's rigorous standards applicable to all APIs manufactured in the U.S. APIs from other sources are subject to detention without physical examination. The agency will continue to work with state regulators, monitor the market, and take enforcement actions as necessary to prevent unsafe or fraudulent GLP-1 drugs from reaching U.S. consumers.[72646]
For storage information, see the specific product information within the How Supplied section.
Ozempic Pen
General information
Subcutaneous Pen Administration (Ozempic Pen)
Wegovy Pen
General information
Subcutaneous Pen Administration (Wegovy Pen)
In monotherapy trials with semaglutide injection for type 2 diabetes mellitus (T2DM), severe hypoglycemia (requiring the assistance of another person) was not reported in either the treatment group or the placebo group. Documented symptomatic hypoglycemia (glucose of 70 mg/dL or less) was reported in 1.6% to 3.8% of subjects receiving semaglutide injection vs. 0% of subjects receiving placebo. Severe or blood glucose confirmed symptomatic hypoglycemia (glucose of 56 mg/dL or less) was not reported in any of the subjects receiving semaglutide monotherapy compared to 1.6% of subjects receiving placebo. In trials where semaglutide was added on to basal insulin with or without metformin, severe hypoglycemia (requiring the assistance of another person) was reported in 1.5% of semaglutide-treated subjects. Documented symptomatic hypoglycemia (glucose of 70 mg/dL or less) was reported in 16.7% to 29.8% of subjects receiving semaglutide, and severe or blood glucose confirmed symptomatic hypoglycemia (glucose of 56 mg/dL or less) was reported in 8.3% to 10.7% of subjects receiving semaglutide. Hypoglycemia was more frequent when semaglutide was used in combination with a sulfonylurea; severe hypoglycemia occurred in 0.8% and 1.2% of subjects when semaglutide 0.5 mg and 1 mg, respectively, was given with a sulfonylurea. In addition, documented symptomatic hypoglycemia occurred in 17.3% and 24.4% of subjects and severe or blood glucose confirmed symptomatic hypoglycemia (glucose of 56 mg/dL or less) occurred in 6.5% and 10.4% of subjects when semaglutide 0.5 mg and 1 mg, respectively, was given with a sulfonylurea.[62656] In monotherapy trials with semaglutide oral tablets for T2DM, severe hypoglycemia (requiring the assistance of another person) was reported in 1% of subjects receiving the 7 mg tablets and 0% of subjects receiving the 14 mg tablets or placebo. A blood glucose level of 54 mg/dL or less occurred in 1% of subjects receiving placebo and 0% of the semaglutide oral treatment groups. Severe hypoglycemia was not reported in any subjects enrolled in trials where semaglutide tablets were added on to metformin and/or sulfonylurea, basal insulin alone, or metformin in combination with basal insulin in subjects with moderate renal impairment. In contrast, blood glucose level of 54 mg/dL or less occurred in 6% of subjects receiving the 14 mg tablets and 3% of subjects receiving placebo. In trials when semaglutide was added on to insulin with or without metformin, severe hypoglycemia was reported in 1% of subjects receiving the 14 mg tablets, 1% of subjects receiving placebo, and 0% of the subjects receiving the 7 mg tablets. A blood glucose level of 54 mg/dL or less was reported in 26% of subjects receiving the 7 mg tablets, 30% of subjects receiving the 14 mg tablets, and 32% with placebo.[64637] In a trial of subjects with T2DM and a BMI of 27 kg/m2 or greater being treated with semaglutide injection for weight loss, clinically significant hypoglycemia (plasma glucose less than 54 mg/dL) was reported in 6.2% of semaglutide-treated subjects versus 2.5% of placebo-treated subjects. A higher rate of clinically significant hypoglycemic episodes was reported with the semaglutide 2.4 mg/week dose versus the 1 mg/week dose (10.7 vs. 7.2 episodes per 100 patient years of exposure, respectively); the rate in the placebo-treated group was 3.2 episodes per 100 patient years of exposure. In addition, 1 episode of severe hypoglycemia requiring intravenous glucose was reported in a semaglutide-treated subject. The risk of hypoglycemia was increased when semaglutide was used with a sulfonylurea. In a cardiovascular outcomes trial in adults without T2DM, 3 episodes of serious hypoglycemia were reported in semaglutide-treated subjects compared to 1 episode in placebo-treated subjects. Subjects with a history of bariatric surgery, a risk factor for hypoglycemia, had more events of serious hypoglycemia while taking semaglutide (2.3%) compared to placebo (0%).[66713]
As with other GLP-1 analogs, gastrointestinal (GI) events are the most commonly reported adverse effects with semaglutide. More subjects receiving semaglutide discontinued treatment due to GI adverse reactions than subjects receiving placebo during all clinical trials. The following adverse effects were reported in subjects receiving semaglutide injection or oral tablets across all clinical trials and at incidences higher than with placebo: nausea (11% to 44%), vomiting (5% to 36%), diarrhea (8.5% to 30%), abdominal pain (5.7% to 20%), abdominal distention (2% to 7%), constipation (3.1% to 24%), dyspepsia (0.6% to 9%), decreased appetite (6% to 9%), eructation (0.6% to 7%), flatulence (0.4% to 6%), gastroesophageal reflux disease (1.5% to 5%), gastroenteritis (4% to 7%), and gastritis (0.4% to 4%). The majority of reports of nausea, vomiting, and/or diarrhea occurred during dose escalation. Appendicitis was reported in 10 (0.5%) semaglutide-treated subjects vs. 2 (0.2%) placebo-treated subjects during clinical trials of semaglutide injection used for weight management. In the trial with semaglutide 1 mg and 2 mg injection for type 2 diabetes mellitus, GI events occurred more frequently among subjects receiving semaglutide 2 mg injection (34%) compared to semaglutide 1 mg injection (30.8%). Severe GI adverse reactions including ileus, GI obstruction, and severe constipation including fecal impaction were reported during postmarketing experience.[62656] [66713] Ileus was also reported during postmarketing experience with oral semaglutide.[64637] Additionally, hemorrhoids and hiccups have also been reported in clinical trials with semaglutide injection for weight management.[62656] [64637] [66713]
Acute gallbladder disease events, such as cholecystitis or cholelithiasis, have been reported in clinical studies with semaglutide. In clinical trials of semaglutide injection for type 2 diabetes mellitus (T2DM), cholelithiasis was reported in 1.5% and 0.4% of adults treated with semaglutide 0.5 mg and 1 mg subcutaneous injection, respectively. Cholelithiasis was not reported with placebo.[62656] In clinical trials of oral semaglutide for T2DM, cholelithiasis was reported in 1% of oral semaglutide 7 mg recipients. Cholelithiasis was not reported with 14 mg oral semaglutide or placebo.[64637] In clinical trials of semaglutide injection for weight management in adults, cholelithiasis was reported in 1.6% and cholecystitis was reported in 0.6% of semaglutide-treated subjects. In clinical trials of semaglutide injection for weight management in pediatric individuals receiving semaglutide, cholelithiasis (3.8%) and cholecystitis (0.8%) were reported. Substantial or rapid weight loss can increase the risk of cholelithiasis; however, the incidence of acute gallbladder disease was greater in semaglutide-treated subjects than in placebo-treated subjects, even after accounting for the degree of weight loss.[66713] Cholecystectomy has been reported postmarketing.[62656] During clinical trials in adolescents 12 years and older, elevated hepatic enzymes (increased alanine aminotransferase [ALT]) 5 times the upper limit of normal (ULN) or greater were observed in 3% of semaglutide-treated subjects. In some subjects, increases in ALT and AST were associated with other confounding factors (i.e., gallstones). Additionally, in a cardiovascular outcomes trial in adults without T2DM, hyperbilirubinemia (total bilirubin of 3 or more times the ULN) was reported in 0.3% of semaglutide-treated subjects.[66713]
In placebo-controlled trials of semaglutide injection for type 2 diabetes mellitus (T2DM), fatigue, dysgeusia, and dizziness were reported in greater than 0.4% of semaglutide-treated subjects.[62656] Dysgeusia (1.7%) was also reported in clinical trials with semaglutide injection for weight management.[66713] In placebo-controlled trials of semaglutide injection for weight management, headache (14% to 17%), fatigue (11%), dizziness (8%), and anxiety (4%) were reported in treated subjects.[66713] Suicidal behavior and suicidal ideation have been reported in clinical trials with other incretin mimetics indicated for weight management. Monitor people for the emergence or worsening of depression, suicidal thoughts or behavior, and any unusual changes in moods or behaviors. Discontinue semaglutide in people who develop suicidal thoughts or behaviors.[66713] In January 2024, the FDA announced that they have not found evidence that use of GLP-1 receptor agonists (RAs) for T2DM or weight management causes suicidal thoughts or actions. During their preliminary evaluation, they conducted detailed reviews of reports of suicidal thoughts or actions received in the FDA Adverse Event Reporting System (FAERS) and reviews of clinical trials, including large outcome studies and observational studies. However, because of the small number of suicidal thoughts or actions observed in both people using GLP-1 RAs and in the comparative control groups, they cannot definitively rule out that a small risk may exist; therefore, FDA is continuing to look into this issue. Further evaluations include a meta-analysis of clinical trials across all GLP-1 RA products and an analysis of postmarketing data in the Sentinel System; final conclusions and recommendations will be communicated once more information is known.[70130]
In placebo-controlled trials for type 2 diabetes mellitus, an injection site reaction (e.g., injection-site discomfort, erythema) was reported in 0.2% of subjects receiving semaglutide. In clinical trials, 1.4% of subjects treated with semaglutide injection for weight management experienced injection site reactions (including injection site pruritus, erythema, inflammation, induration, and irritation) vs. 1% with placebo.[62656] [66713]
Antibody formation against semaglutide has been reported. In clinical trials with semaglutide injection for type 2 diabetes mellitus (T2DM), 32 (1%) subjects receiving semaglutide tested positive for anti-semaglutide antibodies. Of these 32 semaglutide-treated subjects that developed anti-semaglutide antibodies, 19 subjects (0.6% of the overall population) developed antibodies cross-reacting with native GLP-1.[62656] In clinical trials with semaglutide oral tablets for T2DM, 14 (0.5%) subjects developed anti-semaglutide antibodies. Of the 14 semaglutide-treated subjects that developed anti-semaglutide antibodies, 7 subjects (0.2% of the overall population) developed antibodies cross-reacting with native GLP-1.[64637] In clinical trials with semaglutide injection for weight management, 50 (3%) subjects receiving semaglutide tested positive for anti-semaglutide antibodies. Of these 50 semaglutide-treated subjects that developed anti-semaglutide antibodies, 28 subjects (2% of the overall population) developed antibodies cross-reacting with native GLP-1. In subjects with noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH), 0.4% of subjects developed anti-semaglutide antibodies which were also cross-reactive to native GLP-1.[66713] The in vitro neutralizing activity of the antibodies is uncertain at this time. The incidence of antibodies to semaglutide cannot be directly compared with the incidence of antibodies of other products.[62656] [64637] [66713]
There have been postmarketing reports of acute renal failure, in some cases requiring hemodialysis, in people treated with semaglutide. The majority of the reported events occurred in subjects who experienced gastrointestinal reactions leading to dehydration such as nausea, vomiting, or diarrhea. In clinical trials of semaglutide injection for weight management, acute kidney injury occurred in 7 subjects (0.4 cases per 100 patient years) receiving semaglutide vs. 4 subjects (0.2 cases per 100 patient years) receiving placebo. The risk of renal adverse reactions was increased in subjects with a history of renal impairment (the weight management trials included 65 subjects with a history of moderate or severe renal impairment at baseline), and occurred more frequently during dose titration. Monitor renal function in people reporting adverse reactions to semaglutide that could lead to volume depletion, especially during dosage initiation and escalation.[62656] [64637] [66713] In a cardiovascular outcomes trial involving adults without type 2 diabetes mellitus, urolithiasis was reported in 1.2% of semaglutide-treated subjects vs. 0.8% of placebo-treated subjects, including serious reactions that were reported more frequently in subjects receiving semaglutide (0.6%) vs. placebo (0.4%).[66713]
In clinical trials of semaglutide for type 2 diabetes mellitus (T2DM), subjects exposed to semaglutide subcutaneous injection reported increases in amylase (hyperamylasemia) and lipase, and had a mean increase from baseline in amylase of 13% and lipase of 22%. These changes were not observed in placebo-treated subjects.[62656] In trials with semaglutide oral tablets, subjects exposed to semaglutide 7 mg and 14 mg oral tablets had a mean increase from baseline in amylase of 10% and 13%, respectively, and lipase of 30% and 34%, respectively. These changes were not observed in placebo-treated subjects.[64637] In clinical trials of semaglutide injection for weight management, subjects treated with semaglutide had a mean increase from baseline in amylase of 15% to 16% and lipase of 39%. These changes were not observed in the placebo group. During clinical trials, adults with noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH) had increases in lipase greater than 3 times the upper limit of normal occurred in 4.7% (35/750) of semaglutide-treated subjects compared with 1.3% (5/374) of placebo treated subjects.[66713] There have been reports of acute pancreatitis in people taking semaglutide during premarketing trials. In glycemic control trials with semaglutide injection, acute pancreatitis was reported in 7 semaglutide-treated subjects (0.3 cases per 100 patient years) vs. 3 in comparator-treated subjects (0.2 cases per 100 patient years). One case of chronic pancreatitis was confirmed in a semaglutide-treated subject. In a 2-year trial, acute pancreatitis was reported in 8 semaglutide-treated subjects (0.27 cases per 100 patient years) and 10 placebo-treated subjects (0.33 cases per 100 patient years), both on a background of standard of care.[62656] Subjects receiving oral semaglutide in clinical trials, pancreatitis was reported as a serious adverse event in 6 subjects (0.1 events per 100 patient years) receiving semaglutide versus 1 in comparator-treated subjects (less than 0.1 events per 100 patient years).[64637] In clinical trials of semaglutide injection for weight management, acute pancreatitis was confirmed by adjudication in 4 semaglutide-treated subjects (0.2 cases per 100 patient years) versus 1 in placebo-treated subjects (less than 0.1 cases per 100 patient years). One additional case of acute pancreatitis was confirmed in a subject treated with semaglutide in another clinical trial.[66713] The FDA and the EMA have stated that after review of published and unpublished reports, the current data do not support an increased risk of pancreatitis and pancreatic cancer in people receiving incretin mimetics. The agencies have not reached any new conclusions about safety risks of the incretin mimetics, although they have expressed that the totality of the data that have been reviewed provides reassurance. Continue to consider precautions related to pancreatic risk until more data are available.[53573] [56778] After treatment initiation and dose increases, people should be observed carefully for signs and symptoms of pancreatitis (which may include persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by nausea or vomiting). Discontinue semaglutide and initiate appropriate management if pancreatitis is suspected. Semaglutide for T2DM has not been studied in subjects with a history of pancreatitis.[62656] [64637] [66713]
During a clinical trial in pediatric subjects 12 years and older receiving semaglutide for weight management, rash (3%) and urticaria (3%) were reported. Hypersensitivity reactions, including anaphylaxis, anaphylactoid reactions, angioedema, rash, and urticaria, have been reported postmarketing with use of semaglutide.[62656] [64637] [66713]
Sinus tachycardia was observed during clinical studies of semaglutide injection for weight management; mean increases in resting heart rate of 1 to 4 beats per minute (bpm) were seen with routine clinical monitoring in semaglutide-treated subjects vs. placebo. More subjects treated with semaglutide than with placebo had maximum changes from baseline at any visit of 10 to 19 bpm (41% vs. 34%, respectively) and 20 bpm or more (26% vs. 16%, respectively). In a clinical trial of pediatric subjects aged 12 years and older, more subjects treated with semaglutide compared to placebo had maximum changes in heart rate of 20 bpm or more (54% vs. 39%). In placebo-controlled trials for type 2 diabetes mellitus (T2DM), semaglutide injection 0.5 and 1 mg resulted in a mean increase in heart rate of 2 to 3 bpm. There was a mean decrease in heart rate of 0.3 bpm in placebo-treated subjects. In placebo-controlled trials of oral semaglutide for T2DM, semaglutide 7 and 14 mg resulted in a mean increase in heart rate of 2 to 3 bpm. There was no change in heart rate in placebo-treated subjects. Heart rate should be monitored at regular intervals consistent with usual clinical practice in people taking semaglutide and people should inform health care providers of palpitations or feelings of a racing heartbeat while at rest during semaglutide treatment. For people who experience a sustained increase in resting heart rate while taking semaglutide, the drug should be discontinued.[62656] [64637] [66713] Adverse reactions related to hypotension (hypotension, orthostatic hypotension, and decreased blood pressure) were reported in 1.3% to 2.3% of semaglutide-treated subjects vs. 0% to 0.4% of placebo-treated subjects during clinical trials of semaglutide injection for weight management. Syncope was reported in 0.8% and 0.2% of subjects, respectively. Some reactions were related to gastrointestinal adverse reactions and volume loss associated with semaglutide. In adult subjects, hypotension and orthostatic hypotension were more frequently seen in people on concomitant antihypertensive therapy.[66713]
Hair loss (alopecia) was reported in 3% to 4% of subjects receiving semaglutide injection for weight management during clinical trials vs. 0% to 1% of subjects receiving placebo. Alopecia has also been reported with postmarketing experience with semaglutide.[64637] [62656] [66713]
Rapid improvement in glucose control has been associated with a temporary worsening of diabetic retinopathy. In a 2-year trial involving subjects with type 2 diabetes mellitus (T2DM) and high cardiovascular risk, more events of diabetic retinopathy complications occurred in the subjects treated with semaglutide injection (3%) compared to placebo (1.8%). The absolute risk increase for diabetic retinopathy complications was greater among subjects with a history of diabetic retinopathy at baseline (semaglutide 8.2%, placebo 5.2%) than among subjects without a known history of diabetic retinopathy (semaglutide 0.7%, placebo 0.4%).[62656] In a pooled analysis of glycemic control trials with oral semaglutide for T2DM, diabetic retinopathy complications occurred in 4.2% of subjects receiving semaglutide vs. 3.8% with comparator.[64637] In a trial of subjects with T2DM and BMI 27 kg/m2 or more receiving semaglutide injection for weight management, retinal disorders were reported by 6.9% of subjects treated with semaglutide 2.4 mg/week, 6.2% of subjects treated with semaglutide 1 mg/week, and 4.2% of subjects treated with placebo. The majority of events were reported as diabetic retinopathy (4%, 2.7%, and 2.7%, respectively) and non-proliferative retinopathy (0.7%, 0%, and 0%, respectively).[66713] The effect of long-term glycemic control with semaglutide on diabetic retinopathy complications has not been studied. People with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy during treatment.[62656] [64637] [66713]
Semaglutide may be associated with the development of a new primary malignancy. Nonclinical studies in rodents of clinically relevant doses of GLP-1 receptor agonists showed dose-related and treatment-duration-dependent increases in the incidence of thyroid C-cell tumors (adenomas and carcinomas). It is unknown whether GLP-1 receptor agonists are associated with thyroid C-cell tumors, including MTC in humans. Cases of MTC in subjects treated with liraglutide, another GLP-1 receptor agonist, have been reported in the postmarketing period; the data in these reports are insufficient to establish or exclude a causal relationship between MTC and GLP-1 receptor agonist use in humans. In clinical trials, there were 7 reported cases of papillary thyroid carcinoma in subjects treated with liraglutide and 1 case in a comparator-treated subject (1.5 vs. 0.5 cases per 1,000 patient years). Most of these papillary thyroid carcinomas were less than 1 cm in greatest diameter and were diagnosed after thyroidectomy, which was prompted by finding on protocol-specified screening with serum calcitonin or thyroid ultrasound.[38653] People should be counseled on the risk and symptoms of thyroid tumors (e.g. symptoms may include a mass in the neck, dysphagia, dyspnea or persistent hoarseness). Although routine monitoring of serum calcitonin is of uncertain value in people treated with semaglutide, if serum calcitonin is measured and found to be elevated, the individual should be referred to an endocrinologist for further evaluation.[62656] [64637] [66713]
During a clinical trial in pediatric subjects 12 years and older receiving semaglutide for weight management, naso-pharyngitis (12% vs. 10% placebo), sinusitis (4% vs. 2% placebo), urinary tract infection (4% vs. 2% placebo), and influenza (3% vs. 0% placebo) were reported. Ligament sprain was reported in 4% of pediatric subjects 12 years and older receiving semaglutide for weight management compared to 2% of subjects receiving placebo.[66713]f
In clinical trials with semaglutide injection for weight management, dysesthesia, which includes paresthesias, hyperesthesia, burning sensation/skin burning sensation, allodynia, skin pain, and sensitive skin, was reported in 2% of semaglutide-treated subjects compared to 1% placebo.[66713]
In a cardiovascular outcomes trial of adults without type 2 diabetes mellitus, bone fractures (e.g., hip and pelvis fractures) were reported more frequently in adult females and adults aged 75 years and older taking semaglutide (1% and 2.4%, respectively) compared to placebo (0.2% and 0.6%, respectively). In a clinical trial in adults with noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH), fractures occurred in 4.4% of subjects (2.6 cases per 100 patient years) compared to placebo (3.3%; 2 cases per 100 patient years). Fractures were reported in both males and females with a median age of 61 years (range, 44 to 75 years).[66713]
There have been postmarketing reports of perioperative pulmonary aspiration in people receiving GLP-1 receptor agonists who underwent elective surgery or procedures requiring general anesthesia or deep sedation. Despite adherence to preoperative fasting guidelines, these subjects were found to have residual gastric contents. The available data is insufficient to give recommendations on mitigating the risk of pulmonary aspiration during general anesthesia or deep sedation in people taking semaglutide, including whether to modify preoperative fasting recommendations or temporarily discontinue semaglutide.[62656] [64637] [66713]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Anaphylaxis and angioedema have been reported with GLP-1 receptor agonists. Use semaglutide with caution in people with a history of angioedema or anaphylaxis with another GLP-1 receptor agonist because it is unknown whether such individuals will be predisposed to these reactions with semaglutide.[62656][64637][66713]
Semaglutide is contraindicated in patients with a personal or family history of certain types of thyroid cancer, specifically thyroid C-cell tumors such as medullary thyroid carcinoma (MTC), or in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2). Semaglutide has been shown to cause dose-dependent and treatment duration-dependent malignant thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. A statistically significant increase in cancer was observed in rats receiving semaglutide at all dose levels (greater than 2X human exposure). It is unknown whether semaglutide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans. Patients should be counseled on the potential risk and symptoms of thyroid tumors (e.g. a mass in the neck, dysphagia, dyspnea or persistent hoarseness). Although routine monitoring of serum calcitonin is of uncertain value in patients treated with semaglutide, if serum calcitonin is measured and found to be elevated, the patient should be referred to an endocrinologist for further evaluation.[62656] [64637] [66713]
Because semaglutide is commonly associated with GI adverse reactions which are sometimes severe, including slowed gastric emptying, nausea, vomiting, and diarrhea, the use of semaglutide is not recommended in people with severe gastroparesis.[62656] [64637] [66713]
During semaglutide therapy, people with a history of diabetic retinopathy should be closely monitored. Inform semaglutide recipients to contact their care team if changes in vision are experienced during treatment. There is an increased risk for diabetic retinopathy complications in people with a history of diabetic retinopathy at baseline compared to those without a known history of diabetic retinopathy. Rapid improvement in glucose control has been associated with a temporary worsening of diabetic retinopathy. The effect of long-term glycemic control with semaglutide on diabetic retinopathy complications has not been studied.[62656] [64637] [66713]
Semaglutide may be associated with reproductive risk and preconceptual planning is recommended; people who may become pregnant should discontinue semaglutide at least 2 months before a planned pregnancy due to the drug's long washout period.[62656] [64637] [66713]
Use injectable semaglutide with caution during lactation; oral semaglutide therapy is not recommended during breast-feeding.[62656] [64637] [66713] A clinical lactation study reported semaglutide concentrations below the lower limit of quantification in human breast milk.[64637] However, salcaprozate sodium (SNAC) (an absorption enhancer in oral semaglutide tablets) and/or its metabolites concentrated in the milk of lactating rats. There are no data on the presence of SNAC in human milk. Since the activity of UGT2B7, an enzyme involved in SNAC clearance, is lower in infants compared to adults, higher SNAC plasma levels may occur in neonates and infants. Because of the unknown potential for serious adverse reactions in the breastfed infant due to the possible accumulation of SNAC from breast-feeding and because semaglutide injection can be considered for use during lactation, breast-feeding is not recommended during treatment with oral semaglutide tablets.[64637] If semaglutide is discontinued in an individual with type 2 diabetes mellitus and blood glucose is not controlled on diet and exercise alone, insulin therapy may be considered. Oral hypoglycemics may also be considered. Metformin monotherapy may be appropriate for some patients as available studies indicate low excretion in milk and that maternal use during breast-feeding is not expected to result in side effects to a healthy nursing infant. Some experts recommend using metformin with caution if the patient is breastfeeding a newborn or a premature neonate with reduced renal function.[31407] [31408] [31409] [32459] [70364] Because acarbose has limited systemic absorption, which results in minimal maternal plasma concentrations, clinically significant exposure via breast milk is not expected; therefore, this agent may be an alternative if postprandial glucose control is needed.[46303] Glyburide may be a suitable alternative since it was not detected in the breast milk of lactating women who received single and multiple doses of glyburide.[31568] If any oral hypoglycemics are used during breast-feeding, the nursing infant should be monitored for signs of hypoglycemia, such as increased fussiness or somnolence.[46104]
Avoid semaglutide products for weight management in people with a history of suicidal attempts or active suicidal ideation; use it with caution in people with a history of depression. Suicidal behavior and ideation have been reported in clinical trials with other weight management products. Monitor recipients of semaglutide for weight management for the emergence or worsening of depression, suicidal thoughts or behaviors, and/or any unusual changes in mood or behavior. Discontinue semaglutide products for weight management in people who experience suicidal thoughts or behaviors.[66713] In January 2024, the FDA announced that they have not found evidence that use of GLP-1 receptor agonists (RAs) for type 2 diabetes or weight management causes suicidal thoughts or actions. During their preliminary evaluation, they conducted detailed reviews of reports of suicidal thoughts or actions received in the FDA Adverse Event Reporting System (FAERS) and reviews of clinical trials, including large outcome studies and observational studies. However, because of the small number of suicidal thoughts or actions observed in both people using GLP-1 RAs and in the comparative control groups, they cannot definitively rule out that a small risk may exist; therefore, FDA is continuing to look into this issue. Further evaluations include a meta-analysis of clinical trials across all GLP-1 RA products and an analysis of postmarketing data in the Sentinel System; final conclusions and recommendations will be communicated once more information is known.[70130]
Use semaglutide with caution in people with a history of pancreatitis. After initiation of semaglutide, observe people carefully for signs and symptoms of pancreatitis (which may include persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by nausea or vomiting). Acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in people treated with GLP-1 receptor agonists, including semaglutide. If pancreatitis is suspected, discontinue semaglutide promptly and initiate appropriate management.[62656] [64637] [66713]
Semaglutide (Wegovy) for the treatment of obesity or weight management should not be used during pregnancy because weight loss offers no potential benefit to a pregnant individual and may result in fetal harm due to the potential hazard of maternal weight loss to the fetus. Semaglutide (Wegovy) should be used with caution for the treatment of noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH) during pregnancy and should be used only if the potential benefit justifies the potential risk to the fetus. There may be risks to the mother and fetus related to underlying MASH with advanced liver fibrosis (e.g., increased risks of gestational diabetes, hypertensive complications, preterm birth, and postpartum hemorrhage). Whether semaglutide treatment during pregnancy reduces these risks is unknown. Discontinue semaglutide at least 2 months before a planned pregnancy, in order to account for a long washout period for semaglutide. There is a pregnancy exposure registry for women who use semaglutide intended for weight management (Wegovy) during pregnancy. Contact Novo Nordisk at 1-877-390-2760 or www.wegovypregnancyregistry.com for more information.[66713] There are no adequate data or clinical studies of semaglutide use for the treatment of type 2 diabetes mellitus (T2DM) during pregnancy to inform a drug-associated risk for adverse developmental outcomes; use in pregnancy only if the potential benefit justifies the potential risk to the fetus. Rat studies have noted embryofetal mortality, structural abnormalities, and alterations to growth at maternal exposures below the maximum recommended human dose (MRHD) based on exposure AUC. In rabbits and cynomolgus monkeys administered semaglutide during organogenesis, early pregnancy losses and structural abnormalities were observed at below the MRHD (rabbit) and 5-fold or greater the MRHD (monkey). Poorly controlled diabetes during pregnancy also increases fetal risk.[62656] [64637] In addition, salcaprozate sodium (SNAC), an absorption enhancer in oral semaglutide tablets, crosses the placenta, and reaches fetal tissues in rats. In a pre- and postnatal development study of SNAC exposure, an increase in gestation length, an increase in the number of stillbirths, and a decrease in pup viability were observed.[64637] The American College of Obstetricians and Gynecologists (ACOG) and the American Diabetes Association (ADA) continue to recommend human insulin as the standard of care in pregnant women with diabetes mellitus and gestational diabetes mellitus (GDM) requiring medical therapy; insulin does not cross the placenta.[64926] [62358] [62656] [64637]
Semaglutide an incretin mimetic; specifically, semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist with 94% sequence homology to human GLP-1. Semaglutide binds and activates the GLP-1 receptor. The principal mechanism of protraction resulting in the long half-life of semaglutide is albumin binding, which results in decreased renal clearance and protection from metabolic degradation; semaglutide is stabilized against degradation by the DPP-4 enzyme. Semaglutide reduces blood glucose through a mechanism where it stimulates insulin secretion and lowers glucagon secretion, both in a glucose-dependent manner. Therefore, when blood glucose is high, insulin secretion is stimulated and glucagon secretion is inhibited. The mechanism of blood glucose lowering also involves a minor delay in gastric emptying in the early postprandial phase.[62656][64637] Semaglutide delays gastric emptying, lowers body weight with greater fat mass loss than lean mass loss, and decreases calorie intake. The effects are likely mediated by affecting appetite. Semaglutide stimulates insulin secretion and reduces glucagon secretion in a glucose-dependent manner which can lead to a reduction of blood glucose. For the treatment of noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH), the precise mechanism of action is not fully understood. Histological improvements in steatosis, inflammation, and fibrosis in the liver (which was associated with body weight loss, intermittent periods of reduced food intake, and improvements in relevant biomarkers) were observed in animal models. The relationship between the pathophysiology of MASH in animal models and humans has not been fully established.[66713] The mechanism of kidney-related and cardiovascular (CV) risk reduction has not been established.[62656][64637]
Revision Date: 10/16/2025, 12:21:24 PMSemaglutide is given via subcutaneous or oral administration. The mean estimated Vd is 12.5 L and 8 L after subcutaneous and oral administration, respectively. Semaglutide is more than 99% bound to plasma albumin. The primary route of elimination is metabolism after proteolytic cleavage of the peptide backbone and sequential beta-oxidation of the fatty acid side-chain. The primary excretion routes of semaglutide is via the urine and feces. Approximately 3% of the dose is excreted in the urine as intact semaglutide. The clearance is approximately 0.05 and 0.04 L/hour after subcutaneous and oral administration, respectively. With an elimination half-life of approximately 1 week, semaglutide will be present in the circulation for about 5 weeks after the last dose and up to 7 weeks after the last dose for the treatment of obesity.[62656][64637][66713]
Affected cytochrome P450 isoenzymes and drug transporters: none
Semaglutide is co-formulated with salcaprozate sodium, which facilitates the absorption of semaglutide after oral administration. The absorption of semaglutide primarily occurs in the stomach. Population pharmacokinetics (PK) estimated semaglutide exposure to increase in a dose-proportional manner. The mean population-PK estimated steady-state concentrations after once daily oral administration of 7 and 14 mg were approximately 6.7 nmol/L and 14.6 nmol/L, respectively. After oral administration, maximum concentration of semaglutide is reached 1 hour post-dose. Steady-state exposure is achieved after 4 to 5 weeks. Population-PK estimated absolute bioavailability of semaglutide is approximately 0.4% to 1% after oral administration.[64637]
Oral semaglutide tablets are formulated with salcaprozate sodium (SNAC), an absorption enhancer. UGT2B7 is an enzyme involved in SNAC clearance.[64637]
After subcutaneous administration, maximum concentrations of semaglutide were attained 1 to 3 days post-dose. Similar exposure is achieved with subcutaneous administration of semaglutide in the abdomen, thigh, or upper arm. The absolute bioavailability of subcutaneous semaglutide is 89%.[62656][66713]
Ozempic
The mean population estimated steady-state concentrations after once weekly subcutaneous administration of 0.5 and 1 mg semaglutide were approximately 65 and 123 nanograms/mL, respectively. Steady-state exposures are achieved after 4 to 5 weeks of once-weekly administration. Exposures at the 0.5 and 1 mg dose concentrations were consistent with a dose-proportional increase. In the trial comparing semaglutide 1 and 2 mg, the mean steady-state concentrations were 111.1 and 222.1 nanograms/mL, respectively.[62656]
Wegovy
The average semaglutide steady-state concentration after subcutaneous administration of semaglutide was approximately 75 nmol/L in subjects with either obesity (BMI 30 kg/m2 or more) or overweight (BMI 27 kg/m2 or more). The steady-state exposure of semaglutide increased proportionally with doses up to 2.4 mg subcutaneously once weekly.[66713]
Hepatic impairment does not have any impact on the exposure of semaglutide. The pharmacokinetics of semaglutide were evaluated in subjects with mild, moderate, and severe hepatic impairment compared with subjects with normal hepatic function in studies with either a single dose of 0.5 mg subcutaneous semaglutide or 10 consecutive days of once-daily semaglutide oral tablets.[62656][64637][66713]
Renal impairment does not impact the pharmacokinetics of semaglutide in a clinically relevant manner. This was evident in studies with either a single dose of 0.5 mg subcutaneous semaglutide or 10 consecutive days of once-daily oral doses of semaglutide in subjects with mild, moderate, severe, and end-stage renal disease (ESRD) compared with subjects with normal renal function; this was also shown for subjects with both type 2 diabetes mellitus and renal impairment based on data from clinical studies.[62656][64637][66713]
The pharmacokinetics of semaglutide have not been studied in children.[62656][64637][66713]
Age did not significantly affect the pharmacokinetics of semaglutide.[62656][64637][66713]
Gender did not significantly affect the pharmacokinetics of semaglutide.[62656][64637]
Race did not significantly affect the pharmacokinetics of semaglutide.[62656][64637][66713]
In the clinical trials, the exposure of semaglutide exhibited an indirect relationship with an increase in body weight; however, subcutaneous semaglutide doses of 0.5 and 1 mg provide adequate systemic exposure over the body weight range of 40 to 198 kg.[62656] Oral doses of 7 and 14 mg provide adequate systemic exposure over the body weight range of 40 to 188 kg.[64637]
Upper Gastrointestinal (GI) Disease
Disease in the upper GI tract (chronic gastritis and/or gastroesophageal reflux disease) does not impact semaglutide pharmacokinetics in a clinically relevant manner; this was shown in a study in subjects with type 2 diabetes mellitus with or without upper GI disease given semaglutide oral tablets once daily for 10 consecutive days.[64637]
Noncirrhotic Metabolic Dysfunction-Associated Steatohepatitis (MASH)
Fibrosis stage (F2 or F3) did not impact semaglutide exposure in individuals with MASH. There is no difference observed in the exposure of semaglutide (Wegovy) following subcutaneous administration between individuals with MASH and individuals who are overweight or with obesity.[66713]
Use injectable semaglutide with caution during lactation; oral semaglutide therapy is not recommended during breast-feeding.[62656] [64637] [66713] A clinical lactation study reported semaglutide concentrations below the lower limit of quantification in human breast milk.[64637] However, salcaprozate sodium (SNAC) (an absorption enhancer in oral semaglutide tablets) and/or its metabolites concentrated in the milk of lactating rats. There are no data on the presence of SNAC in human milk. Since the activity of UGT2B7, an enzyme involved in SNAC clearance, is lower in infants compared to adults, higher SNAC plasma levels may occur in neonates and infants. Because of the unknown potential for serious adverse reactions in the breastfed infant due to the possible accumulation of SNAC from breast-feeding and because semaglutide injection can be considered for use during lactation, breast-feeding is not recommended during treatment with oral semaglutide tablets.[64637] If semaglutide is discontinued in an individual with type 2 diabetes mellitus and blood glucose is not controlled on diet and exercise alone, insulin therapy may be considered. Oral hypoglycemics may also be considered. Metformin monotherapy may be appropriate for some patients as available studies indicate low excretion in milk and that maternal use during breast-feeding is not expected to result in side effects to a healthy nursing infant. Some experts recommend using metformin with caution if the patient is breastfeeding a newborn or a premature neonate with reduced renal function.[31407] [31408] [31409] [32459] [70364] Because acarbose has limited systemic absorption, which results in minimal maternal plasma concentrations, clinically significant exposure via breast milk is not expected; therefore, this agent may be an alternative if postprandial glucose control is needed.[46303] Glyburide may be a suitable alternative since it was not detected in the breast milk of lactating women who received single and multiple doses of glyburide.[31568] If any oral hypoglycemics are used during breast-feeding, the nursing infant should be monitored for signs of hypoglycemia, such as increased fussiness or somnolence.[46104]
Semaglutide (Wegovy) for the treatment of obesity or weight management should not be used during pregnancy because weight loss offers no potential benefit to a pregnant individual and may result in fetal harm due to the potential hazard of maternal weight loss to the fetus. Semaglutide (Wegovy) should be used with caution for the treatment of noncirrhotic metabolic dysfunction-associated steatohepatitis (MASH) during pregnancy and should be used only if the potential benefit justifies the potential risk to the fetus. There may be risks to the mother and fetus related to underlying MASH with advanced liver fibrosis (e.g., increased risks of gestational diabetes, hypertensive complications, preterm birth, and postpartum hemorrhage). Whether semaglutide treatment during pregnancy reduces these risks is unknown. Discontinue semaglutide at least 2 months before a planned pregnancy, in order to account for a long washout period for semaglutide. There is a pregnancy exposure registry for women who use semaglutide intended for weight management (Wegovy) during pregnancy. Contact Novo Nordisk at 1-877-390-2760 or www.wegovypregnancyregistry.com for more information.[66713] There are no adequate data or clinical studies of semaglutide use for the treatment of type 2 diabetes mellitus (T2DM) during pregnancy to inform a drug-associated risk for adverse developmental outcomes; use in pregnancy only if the potential benefit justifies the potential risk to the fetus. Rat studies have noted embryofetal mortality, structural abnormalities, and alterations to growth at maternal exposures below the maximum recommended human dose (MRHD) based on exposure AUC. In rabbits and cynomolgus monkeys administered semaglutide during organogenesis, early pregnancy losses and structural abnormalities were observed at below the MRHD (rabbit) and 5-fold or greater the MRHD (monkey). Poorly controlled diabetes during pregnancy also increases fetal risk.[62656] [64637] In addition, salcaprozate sodium (SNAC), an absorption enhancer in oral semaglutide tablets, crosses the placenta, and reaches fetal tissues in rats. In a pre- and postnatal development study of SNAC exposure, an increase in gestation length, an increase in the number of stillbirths, and a decrease in pup viability were observed.[64637] The American College of Obstetricians and Gynecologists (ACOG) and the American Diabetes Association (ADA) continue to recommend human insulin as the standard of care in pregnant women with diabetes mellitus and gestational diabetes mellitus (GDM) requiring medical therapy; insulin does not cross the placenta.[64926] [62358] [62656] [64637]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.